Tools and resources to facilitate family health history collection and assessment.
| The best way to identify red flags is by taking a family history (in addition to a personal health history). |  |
 |
|
 |
|
General family history tools:
A family health history records the health conditions of an individual and their biological relatives (alive and deceased), helping to identify genetic and heritable risks for certain diseases. It is often depicted through a family tree or pedigree.
| |
Important information and questions |
- Try to obtain a three generation history (grandparents, parents, patient’s generation, siblings and cousins or Parents, patient’s generation, their children)
- Ask ages: current age, age at death
- Ask about health conditions, age of onset/diagnosis
 |
|
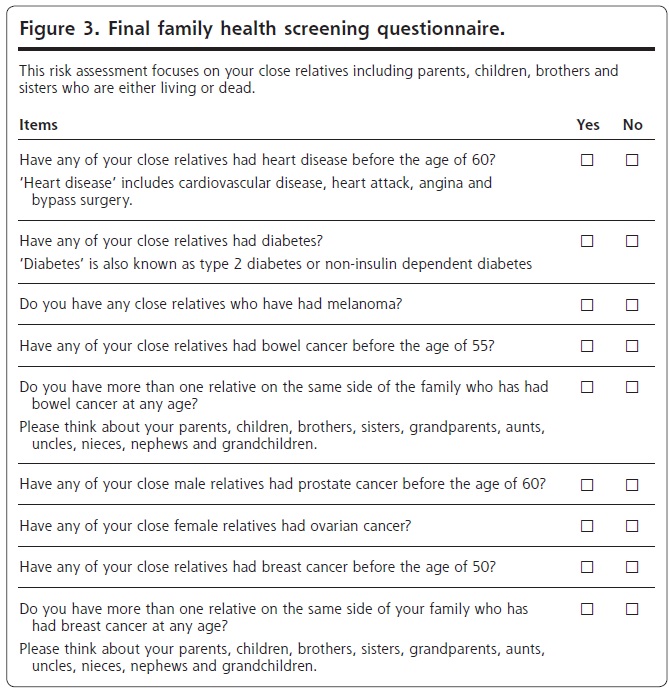 |
Full text available at: https://www.annfammed.org/content/12/3/241.long Posted with permission from Dr. Emery and Reprinted with permission under the CC BY-NC-ND license https://creativecommons.org/licenses/by-nc-nd/4.0/.
|
 |
|
 |
|
 |
|
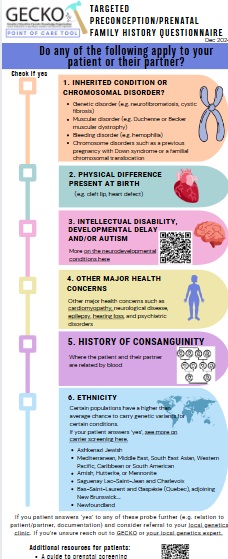
Disease specific tools:
After a general, three-generation family history is obtained, if there are red flags (e.g. multiple affected relatives, young age of diagnosis, see this point of care tool for more) you can use the tools below to complete a more targeted history can help to identify those who may qualify for modified screening (e.g. starting earlier, more frequent, alternate modality), a genetic assessment and/or genetic testing.
Some tools have been developed by GECKO, some are developed by others and are freely available online, and some were developed in collaboration with GECKO as part of a randomized control trial, FHAMe (more on this project below)*.
- Cancer (general)
- Cardiovascular disease
- Diabetes
| |
Cancer |
Characteristics of an individual/family at increased risk of hereditary cancer
 |
|
|
|
Hereditary Breast/Ovarian Cancer
 |
|
 |
|
About 5-10% of breast cancer and about 15% of ovarian cancer is due to inherited genetic change(s). Pathogenic variants in the BRCA1 or BRCA2 genes are the most common cause of hereditary breast and ovarian cancer (HBOC). Pathogenic variants in these genes are associated with a significant increased lifetime risk for breast, ovarian, and other cancers. Additional genes are known to be associated with increased lifetime risk for these cancers and can impact screening and medical management. Genetic testing generally involves a large gene panel where several (>7) genes associated with breast/ovarian in addition to other cancers are analysed.
- While not all individuals will qualify for genetic testing, some will qualify for modified cancer screening and a more appropriate relative (the youngest, affected individual) may be offered genetic testing.
- Individuals with a personal and/or family history that are at high risk (generally >5%) to carry a pathogenic variant in a hereditary breast/ovarian cancer gene can be offered referral to genetic services for a discussion of the benefits, harms and limitations of genetic testing, while women whose family histories suggest a low risk of a hereditary predisposition can be reassured and offered screening following provincial guidelines.
- (For more information see the comprehensive GECKO deep dive or the concise GECKO on the run
Hereditary colorectal/endometrial cancer (Lynch syndrome)
 |
|
 |
|
Lynch syndrome (LS), previously known as hereditary non-polyposis colorectal cancer (HNPCC), is the most common form of hereditary colorectal cancer (CRC) and endometrial cancer (EC), affecting at least 1 in 279 individuals. LS is autosomal dominant. In addition to an increased lifetime risk for colorectal and endometrial cancers, there can be an increased risk for malignancies in the stomach, small bowel, brain, skin and more. Cancer risks and age of onset depend on which LS-associated gene is identified to have a pathogenic/likely pathogenic variant in the individual/family. Individuals suspected of having LS should be referred for a genetic assessment for consideration of genetic testing. Screening, surveillance and management of CRC, EC and other cancers should be guided by genetic test results and/or family/personal history. Studies show that conversations between patients and their healthcare providers are the strongest driver of screening participation. (For more information see the GECKO deep dive or the concise GECKO on the run).
Because of overlap in clinical presentation of hereditary cancer conditions and advances in genomic technology, testing generally involves a large gene panel where several (e.g. >5) genes associated with colorectal and other cancers are analysed.
Prostate cancer
 |
|
Skin cancer
 |
|
Hereditary Renal Cell Cancers
 |
|
Outlines how to identify those patients most likely to benefit from referral to genetics for assessment of a hereditary renal cell cancer syndrome including brief summary of renal cell carcinoma syndromes
Cardiovascular disease
Diabetes
*These family history clinical decision support tools were developed and evaluated as part of the project Family History App in Personalized Medicine (FHAMe). The aim of FHAMe was to determine if an innovative family history strategy will improve healthcare delivery, specifically what proportion of intervention patients have updated documentation of family history in the EMR, and to describe contextual factors that may influence implementation of this novel family history approach into primary care. Manuscripts in preparation.
- Investigators: Carroll JC, Greiver M, Kukan S, Bearss E, Walji S, Moineddin R, Aliarzadeh B, Ivers N, Kalia S, Allanson J, Grunfeld E, Gupta K, Heisey R, Kavanagh D, Kim R, Levy M, Morrison S, Muraca M, Mutasingwa D, O’Brien MA, Permaul J, Sullivan F, Wilson B




