 |
Download this resource in a concise 1-page version or the whole resource (4-pages). |
For a comprehensive guide on prenatal screening including enhanced first trimester screening, next steps following results, more questions to consider, please see this Guide.
*New* Check out this 6-question preconception/prenatal family history screening tool
What is prenatal screening?
Prenatal screening is about checking the health and development of your baby before it is born. It means getting information to better understand the chances of certain health conditions for your baby. Prenatal screening cannot tell you for certain if you baby does or does not have a condition.
Prenatal screening can involve blood work and/or an ultrasound.
 |
This resource is about Non-Invasive Prenatal Testing, also called NIPT. |
Can NIPT hurt me or my baby?
|
No. |
NIPT is a blood test. There is no harm to you or the baby. |
Do I have to have NIPT or any prenatal screening?
|
No. |
Prenatal screening is your choice. While every pregnant person should be offered the choice to have prenatal screening, it is everyone’s personal choice to accept or not. |
Can NIPT tell me if my baby will be healthy?
|
No. |
There is no test to guarantee a healthy baby. NIPT will only look for the chance the baby has one of the specific genetic conditions mentioned below (Down syndrome, trisomy 18, trisomy 13 or a sex chromosome difference). |
When can I have NIPT?
The blood can be drawn anytime after 10 weeks’. Results come back in 7-10 business days. If the blood is drawn too early, the test may not work.
What does NIPT look for?
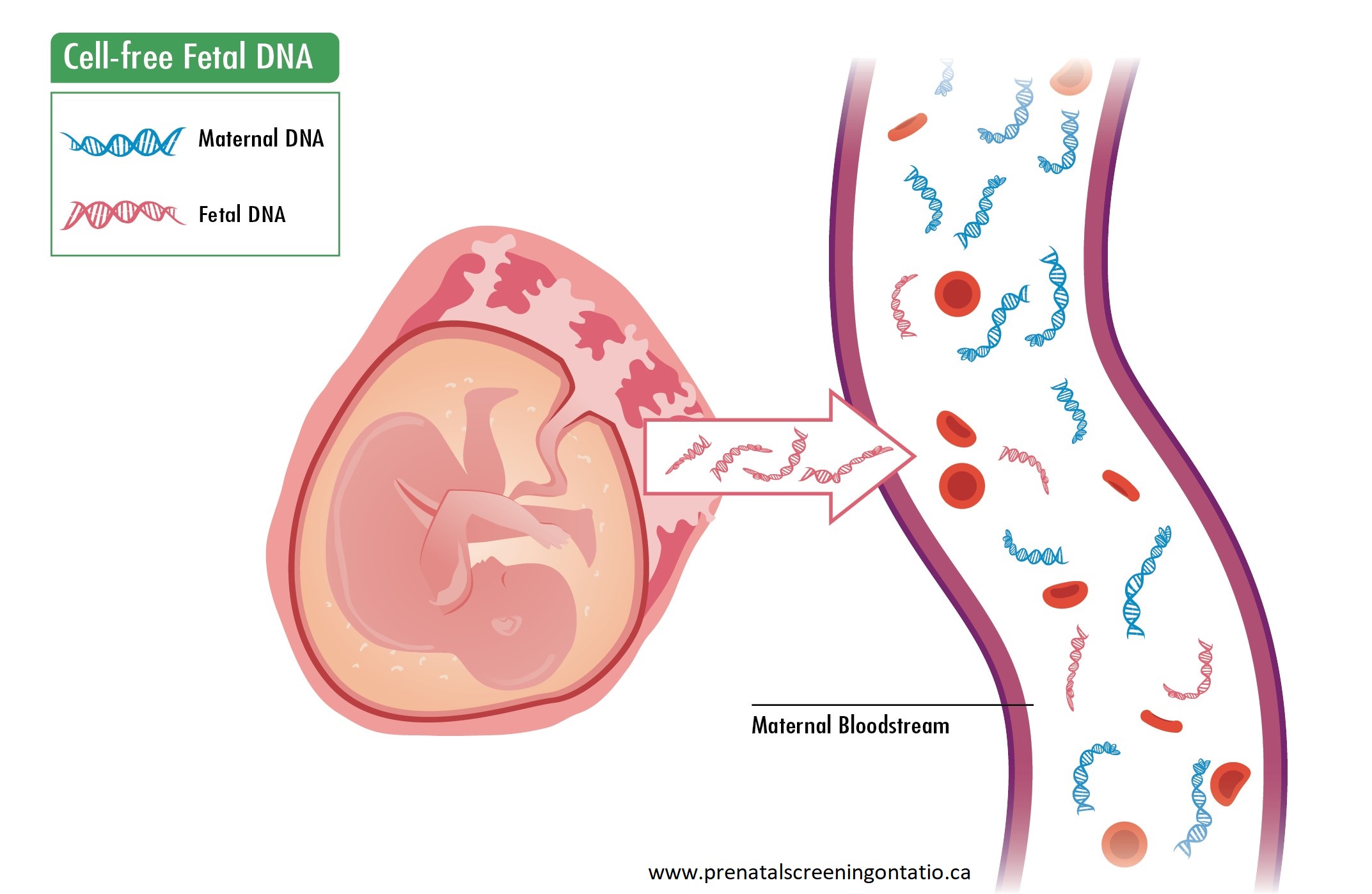
NIPT looks at DNA in your blood. While most (90%) of the DNA in your blood is yours, some (~10%) comes from the pregnancy (specifically, the placenta).
NIPT will report on how likely your baby has a specific genetic condition: Down syndrome, trisomy 18, trisomy 13. Every pregnant person has a chance to have a baby with one of these conditions, and that chance increases with the age of the person (or egg in the case of a donor) when the baby is born. Nobody can cause or prevent these conditions; they occur by chance.
NIPT can also report on the sex chromosomes (male or female). Sometimes NIPT will report that there might be an extra or missing sex chromosome.
A Genetics Minute:
Inside every cell of your body- blood cells, brain cells, heart cells – there is your DNA. This is a library of recipes needed to make important proteins that have jobs for development, maintenance, and health. These ‘recipes’ are called genes. There are about 21,000 genes in your DNA library. The genes are arranged like beads on a string into structures called chromosomes. Typically, a human cell will have 23 pairs of chromosomes numbered 1 to 22, and the 23rd pair are called the sex chromosomes.
Most (99.9%) of the DNA library is the same between person to person, but still this small bit of difference makes each of us unique. Sometimes a difference in our DNA does not have any effect on our health/development, but sometimes a difference as big as a whole extra or missing chromosome containing thousands of genes can have significant effect on health/development.
How good is NIPT?
NIPT will identify almost all pregnancies where the baby has Down syndrome, trisomy 18, or trisomy 13. It is the best screening test to identify Down syndrome.
What will the results say?
The results will most often say that there is a very low chance for the baby to have one of these conditions (less than 0.01% or 1 in 10,000). Sometimes the results will say there is a very high chance the baby has one of the conditions above (higher than 99%). Sometimes the report will say no result which means that the laboratory was not able to get a clear result.
What do I do if the results are low risk?
If your NIPT result is low risk, you can feel reassured that your baby does not have any of the conditions screened for. You will still be offered an ultrasound in the second trimester (18-22 weeks’) to look at your baby’s growth and development.
If there is another reason to suspect a genetic difference in your baby (e.g. something seen on ultrasound or something in your family history), you may still be offered an appointment with a genetics specialist and/or high-risk obstetrician to talk about other testing options.
What do I do if the results are high risk?
If the results are high risk, this does not mean your baby has the condition, but it does means there is a high chance. You will be offered an appointment with a genetics specialist, usually via telephone. Here you will talk about the result, the condition, and next steps such as a diagnostic test to know for sure if your baby does or does not have the condition. Your health care practitioners will support any choice that is right for you.
What do I do if there is no result?
If there is no result, the laboratory might ask that a new blood sample is sent to try again. When this happens, most of the time a result will then be available. Sometimes, it is not possible to get any result from NIPT. In this case, you could be offered an appointment with a genetics specialist to talk about why NIPT can fail and what are possible next steps.
Can NIPT tell me any other information?
Rarely, however because NIPT testing is looking at DNA from both the pregnancy and from you, a result could reveal information about your DNA or health. In these cases, an appointment with a genetics specialist would be offered.
Is there anything else to think about?
Your family history.
Everyone has a chance to have a baby born with a difference or to develop a medical condition, but that chance can be higher if you have a family history of such a difference or medical condition.
If there is something in your family (or pesonal) history - for example a known genetic condition, a close relative* (or personal history) with:
- intellectual disability
- born with one or more differences at birth that needed surgery (like a hole in the heart) or other medical intervention
- young children or babies that passed away unexpectedly or where the cause is not known
- who had more than 3 pregnancy losses
discuss with your healthcare practitioner and a referral for a genetic consultation for you or a relative could be considered.
*A close relative would be a parent, sibling, grandparent, aunt/uncle
Is prenatal screening right for me?
Some questions to consider before NIPT:
- Do I want to know if my baby has one of these conditions before birth?
- What would the results mean for me in this pregnancy?
- Would I consider ending a pregnancy that had one of these conditions?
- Would it be important for me to plan, identify support, and get prepared for a baby that has one of these conditions, before the baby is born?
- Would have a diagnostic test? Would I fly/travel to another city if needed?
- A diagnostic test the only way to know for sure if the baby has the condition before birth (i.e. amniocentesis or chorionic villus sampling). These tests have a small risk to lose the pregnancy (miscarriage).
More on the conditions screened by NIPT:
Down syndrome (also called trisomy 21) is a genetic condition where there is an extra copy of all or a portion of the 21st chromosome. People with Down syndrome are individuals who are as unique and highly variable as anyone else. This extra chromosome usually causes mild to moderate intellectual disability, which means that adults will typically function at the level of an 8–10-year-old. An individual with Down syndrome is expected to learn to read and write and to be physically active, however major developmental milestones will be delayed. Individuals with Down syndrome have a greater possibility of health conditions than the average person, such as heart, stomach, bowel, thyroid, vision and hearing problems. Treatment is available for many of these conditions. There is no way to predict how serious or mild these differences will be. The average life expectancy for a person with Down syndrome is about 60 years. About 1 in 781 babies born has Down syndrome. The chance of having a child with Down syndrome increases with the pregnant person’s age. For more information on Down syndrome, visit the Canadian Down Syndrome Society website.
Trisomy 18 is a genetic condition where there is an extra copy of all or a portion of the 18th chromosome. Every individual with trisomy 18 is different, however serious intellectual disabilities and congenital anomalies that may affect many organ systems (e.g. heart, kidneys) are expected. Many pregnancies with trisomy 18 will miscarry. Most babies born with trisomy 18 do not survive past the first few months of life. About 10% of infants will survive up to 5 years of age, or occasionally longer. Long-term survivors are described as socially interactive with significant physical and intellectual disabilities (e.g. having few words). About 1 in 6,000 babies born has trisomy 18. The chance of having a child with trisomy 18 increases with the pregnant person’s age. For more on trisomy 18, visit The Trisomy 18 Foundation website.
Trisomy 13 is a rare genetic condition where there is an extra copy of all or a portion of the 13th chromosome. Trisomy 13 occurs in approximately 1 in 10,000-25,000 live-born infants. Everyone with trisomy 13 is unique however there is a recognizable pattern of physical differences such as small head, cleft lip and/or palate, small eyes or absent eye as well as serious intellectual disabilities and birth differences that can affect many organ systems (e.g. brain, heart, kidneys). Most pregnancies with trisomy 13 will miscarry. About 5-8% of infants will survive past 1 year. With significant medical intervention longer survival has been reported. For more on trisomy 13, visit The Support Organization for Trisomy 18, 13 and Related Disorders (SOFT) website.
There are several conditions with sex chromosome differences. These types of genetic differences are common and happen in about 1 in 500 individuals. There is a lot of variation between the different conditions depending on which chromosome is extra or missing (X and/or Y). Some features maybe as mild as tall or small height. There may be differences in development such as delayed speech or learning differences. There may be health issues involving puberty or the heart. If your NIPT result reports a high risk for a sex chromosome difference, you will be offered an appointment with a genetics specialist to talk more about the condition and next steps. For more on sex chromosome differences, visit The Association for X and Y Chromosome Variations (AXYS) or the Turner Syndrome Society of Canada for more.
Diagnostic tests
Where screening tests calculate a risk (what is the chance), a diagnostic test will rule in or rule out for sure whether or not a baby has one of the conditions. There are two common diagnostic tests that are offered: chorionic villus sampling (CVS) and amniocentesis. Whereas prenatal screening tests are considered non-invasive as they pose no risk to a pregnancy, diagnostic tests are considered invasive because they are associated with a small procedural risk – an increased chance to lose the pregnancy (miscarriage).
Chorionic villus sampling (CVS)
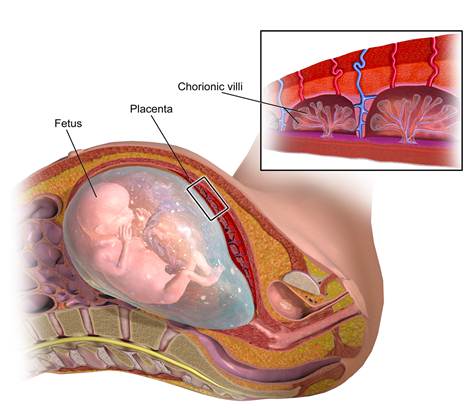 |
What is chorionic villus sampling? Chorionic villus sampling (CVS) is a procedure where a small piece of the placenta is taken and tested. Chorionic villi (see image on the right) attach the placenta to the uterus wall. The placenta is made from the fertilized egg and is expected to have the same genetic information as the baby. CVS is not available in all regions. Talk to your health care practitioner to see if this is an option for you. CVS cannot detect open neural tube defects. When is a CVS carried out? CVS is usually performed between 11 and 13 weeks of pregnancy. |
What is the risk associated with CVS?
Both CVS and amniocentesis have been associated with a slightly increased chance of losing the baby following the procedure (miscarriage). The chance of miscarriage after a CVS or an amniocentesis is 0.5 to 1% (about 1 in 100 or less). Because of the nature of the sample, there is a small chance that the result is difficult to interpret and additional testing, like amniocentesis, may be recommended.
What should I expect at my CVS appointment?
CVS is performed by a specialist in maternal-fetal medicine. You may need to travel to a dedicated hospital if this service is not available near you.
CVS is an outpatient procedure, meaning that you will not need to stay overnight in the hospital. You will be told to have a full bladder. There are two methods to collect a sample from the placenta; either through the vagina or the abdomen. Both methods use ultrasound as a guide the entire time. Through the vagina, using ultrasound, a speculum is inserted (just like a Pap test). Then a very thin, plastic tube is inserted up the vagina and into the cervix. The tube is guided up to the placenta and a small sample is removed. To collect a sample through the abdomen, a thin needle is inserted through the abdominal wall, using ultrasound to guide the needle tip to the placenta.
Will it be painful?
Most people describe the procedure as uncomfortable rather than painful. In general, no medication or anesthetic is given. Through the vagina, the discomfort is similar to that with a Pap test. Through the abdomen, the pain from the needle is similar to having a blood sample drawn. The needle is a bit thicker and a numbing cream may be applied to the skin prior to the procedure. You can expect to experience some uterine cramping during the procedure.
Amniocentesis
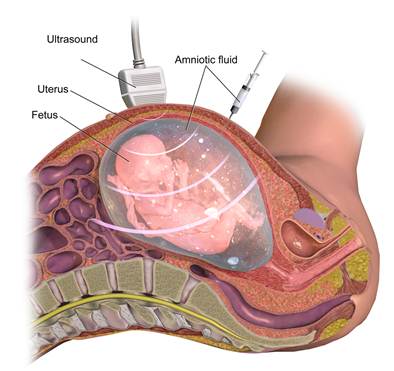 |
What is amniocentesis? Amniocentesis is a procedure where a small sample of amniotic fluid (the fluid that surrounds the baby) is removed and tested. Usually only about 1-2 tablespoons are taken. Amniotic fluid contains fetal cells: skin cells and others cells that are naturally shed by the baby. When is an amniocentesis carried out? The ideal timing is between 15 and 18 weeks to allow opportunity for the procedure, results and decision making. An amniocentesis can, however, be performed any time after 15 weeks. |
What is the risk associated with amniocentesis?
Both CVS and amniocentesis have been associated with a slightly increased chance of losing the baby following the procedure (miscarriage). The chance of miscarriage after a CVS or an amniocentesis is 0.5 to 1% (about 1 in 100 or less).
What should I expect at my amniocentesis appointment?
Amniocentesis is performed by a specialist in maternal-fetal medicine. You may need to travel to a dedicated hospital if this service is not available near you.
Amniocentesis is an outpatient procedure, meaning that you will not need to stay overnight in the hospital. You may be told to have a full bladder, but this will likely depend on how far along in pregnancy you are. To collect a sample of amniotic fluid, using ultrasound guidance the entire time, a thin needle is inserted through the abdominal wall into a pocket of fluid (not near the baby) and fluid is extracted.
Will it be painful?
Most people describe the procedure as uncomfortable rather than painful. In general, no medication or anesthetic is given. The pain from the needle is similar to that when having a blood sample drawn. You can expect to experience some uterine cramping during the procedure.


