Download the PDF here. Download the point of care tool to assist identifying patients most likely to benefit from referral to genetics or the more comprehensive review. Access an education module with case-based learning here.
Bottom line: Long QT syndrome (LQTS) is one of several inherited heart disorders than can lead to sudden cardiac death (SCD). LQTS is a rhythm disorder that can predispose to fast, chaotic heart rhythms which may trigger a sudden fainting spell, seizure or SCD. It is treatable if diagnosed. The ECG is neither sensitive nor specific for hereditary LQTS. A QTc ≥ 500ms is considered high risk for LQTS. Individuals with clinical features such as syncope, and repeated corrected QT interval (QTc) of >450ms for men and >470ms for women, should be referred to a cardiac arrhythmia specialist and a genetics clinic for assessment and genetic testing where indicated. Family physicians can play a crucial role in referring first degree relatives to cardiac genetics specialist services following the death of a young person in whom an autopsy did not identify cause of death or in whom a heritable cardiac disorder was suspected.
Updated Oct 2016
What is long QT syndrome?
Long QT syndrome (LQTS) is a disorder involving the cardiac ion channels resulting in prolongation of the ventricular action potential during cardiac repolarization (i.e. prolonged QT interval on electrocardiogram (ECG)). It occurs in approximately 1 in 2,000 to 1 in 2,500 people. LQTS predisposes to syncope and/or sudden cardiac death and is one of the leading causes of sudden death in otherwise healthy young people. LQTS is one of numerous causes of sudden infant death syndrome (SIDS).
The diagnosis of LQTS usually relies on clinical and family history, in addition to a corrected QT interval (QTc). Determination of an absolute value for an abnormal QTc is difficult as there is a considerable borderline range and the data cut-offs are not clear. Acceptable cut-off values to balance a high positive predictive value and a lowered false positive rate are shown in Table 1.
Table 1. Corrected QT interval (QTc) cut-offs which should prompt referral to cardiac arrhythmia specialists and genetics clinic for assessment [Waddell-Smith et al, 2016].
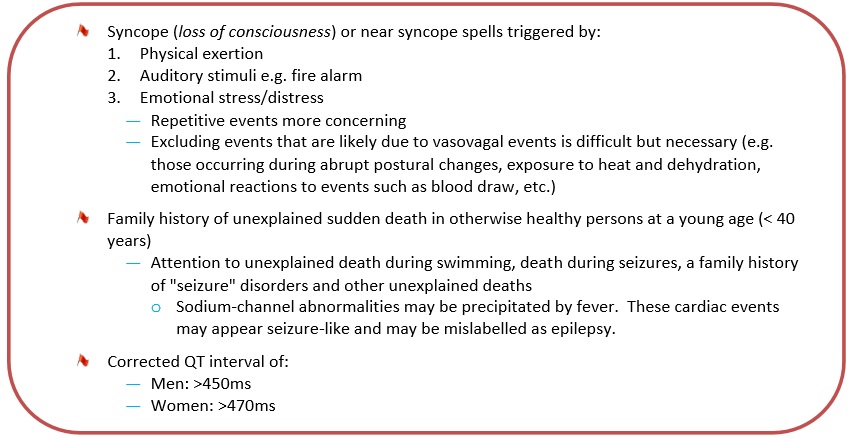
In 20-40% of individuals the ECG may be inconclusive. Since a normal ECG cannot completely “rule out” LQTS, it is recommended that patients be referred to a cardiac specialist for evaluation (which may involve manual calculation of QTc and additional testing) if symptoms, signs or family history are present (Box 1).
Box 1. Clinical symptoms, signs and family history which should prompt referral to cardiac arrhythmia specialists and genetics clinic for assessment.
What do I need to know about the genetics of long QT syndrome?
Most forms of LQTS are hereditary, usually autosomal dominant. LQTS can also be acquired due to other causes such as anorexia nervosa, or induced by certain medications (see Surveillance and Management).
At least 15 genes have been implicated in LQTS. Some genotype-phenotype correlations may be drawn. The three most common genes, accounting for over 90% of known LQTS mutations, are:
- LQT1 (KCNQ1) on chromosome 11, which encodes potassium channel subunits
- LQT2 (HERG, KCNH2) on chromosome 7, which encodes potassium channel subunits
- LQT3 (SCN5A) on chromosome 3, which encodes sodium channel subunits
Red Flags to consider genetic testing or genetic consultation
Consider referral to your local genetics centre for:
Individuals with clinical symptoms (see Box 1) of LQTS or a suggestive ECG
First degree family members of individuals clinically diagnosed with LQTS
First degree relatives of an individual with a known mutation in a LQTS gene
Individuals with a family history of sudden death in a first degree relative under the age of 40
All of the above individuals should also be referred to a cardiac arrhythmia specialist.
Sudden arrhythmic death in the young: other disorders
In addition to LQTS, there are other cardiac disorders, some of them heritable, which can cause sudden death in young people. These include arrhythmogenic and hypertrophic cardiomyopathies, Brugada syndrome and catecholaminergic polymorphic ventricular tachycardia (CPVT). Review of individuals who have experienced cardiac arrest and their first degree relatives may identify a cause in up to~40% of cases. Family physicians may play a crucial role in referring first degree relatives to cardiac genetics specialist services following the death of a young person in whom autopsy did not identify cause of death or in whom a heritable cardiac disorder was suspected. Please refer to Ellison (2015) for an overview of other inherited cardiac disorders that can cause SCD.
What does the genetic test result mean?
LQTS is autosomal dominant. A man or woman with LQTS due to a single faulty gene has a 50% chance of passing the genetic risk for arrhythmia to each child.
LQTS demonstrates reduced penetrance (not every individual who inherits a mutation in a LQTS gene will develop LQTS) and variable expressivity (clinical presentation can vary between affected individuals even within a family).
How will genetic testing help you and your patient?
Genetic testing for LQTS can provide:
- Clarification of LQTS risk status for individuals with borderline clinical investigations
- Identification of individuals in whom a particular mutation confers a higher risk for SCD
- Assistance with life planning (e.g. decisions about careers, participation in competitive sports)
- Relief from worry, for those who test negative for a known family mutation, (a true negative result), as they will not develop the disease in the future and know that their children are not at risk of inheriting the disease
Are there harms or limitations of genetic testing?
Genetic testing can result in:
- Adverse psychological reaction, particularly due to potential for risk of sudden cardiac death, family issues, distress
- Uncertainty due to a genetic variant of unknown significance
- Uncertainty due to limited sensitivity of genetic testing. About 1/4 of LQTS families do not have a recognizable gene mutation
- Insurance/job discrimination
The perceived benefits and limitations of genetic testing may vary with an individual’s personal and family experience of LQTS. The perspective of an individual who has lost a family member to LQTS contrasts significantly with the perspective of an otherwise healthy individual whose prolonged QT interval was picked up incidentally on routine ECG.
Surveillance and management
LQTS is treatable with beta-blockers, implantable cardioverter defibrillators, and avoidance of competitive sports, electrolyte imbalances, and QT-prolonging medications [see www.crediblemeds.org for a comprehensive list (free access, one-time registration required)].
Risk stratification takes into consideration factors such as QTc duration, genotype, gender and age.
For a recent review article on sudden cardiac death see Ellison S. Sudden cardiac death in adolescents. Prim Care Clin Office Pract 2015: 42: 57–76. See online for complete reference list. Other LQTS resource: The Canadian Sudden Arrhythmia Death Syndromes (SADS) Foundation website http://www.sads.ca/
References
Mizusawa Y, Horie M, Wilde AA. Genetic and clinical advances in congenital long QT syndrome. Circ J 2014;78(12):2827-33.
Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes: Document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm 2013;10:1932–63.
Ellison S. Sudden cardiac death in adolescents. Prim Care Clin Office Pract 2015: 42: 57–76.
Gollob MH, Blier L, Brugada R et al. Recommendations for the use of genetic testing in the clinical evaluation of inherited cardiac arrhythmias associated with sudden cardiac death: Canadian Cardiovascular Society. Canadian Heart Rhythm Society joint position paper. Can J Cardiol 2011; 27(2):232-45.
Huisma FF, Potts JE, Gibbs KA, Sanatani S. Assessing the knowledge of sudden unexpected death in the young among Canadian medical students and recent graduates; a cross-sectional study. BMJ Open 2012;2:e001798.
Waddell-Smith KE, Earle N, Skinner JR. Must every child with long QT syndrome take a beta blocker? Arch Dis Child 2015;100(3):279-282.
Waddell-Smith KE, Skinner JR; members of the CSANZ Genetics Council Writing Group. Update on the diagnosis and management of familial long QT syndrome. Heart, Lung and Circulation 2016; 5 (8): 769 –776.
Authors: C Honeywell MSc CCGC, J Rutberg MS CGC, R Gow MBBS FRACP, M Green MD FRCPC, JC Carroll MD CCFP, JE Allanson MD FRCPC and S Morrison MS CGC
Disclaimer:
· GECKO is an independent not-for-profit program that does not accept support from commercial or non-academic entities.
· GECKO aims to aid the practicing non-genetics clinician by providing informed resources regarding genetic/genomic conditions, services and technologies that have been developed in a rigorous and evidence-based manner with periodic updating. The content on the GECKO site is for educational purposes only. No resource should be used as a substitute for clinical judgement. GECKO assumes no responsibility or liability resulting from the use of information contained herein.
· All clinicians using this site are encouraged to consult local genetics clinics, medical geneticists, or specialists for clarification of questions that arise relating to specific patient problems.
· All patients should seek the advice of their own physician or other qualified clinician regarding any medical questions or conditions.
· External links are selected and reviewed at the time a page is published. However, GECKO is not responsible for the content of external websites. The inclusion of a link to an external website from GECKO should not be understood to be an endorsement of that website or the site’s owners (or their products/services).
· We strive to provide accurate, timely, unbiased, and up-to-date information on this site, and make every attempt to ensure the integrity of the site. However, it is possible that the information contained here may contain inaccuracies or errors for which neither GECKO nor its funding agencies assume responsibility.