Download the updated PDF here [2025]
See also the point of care tool for a 2-page summary. ![]()
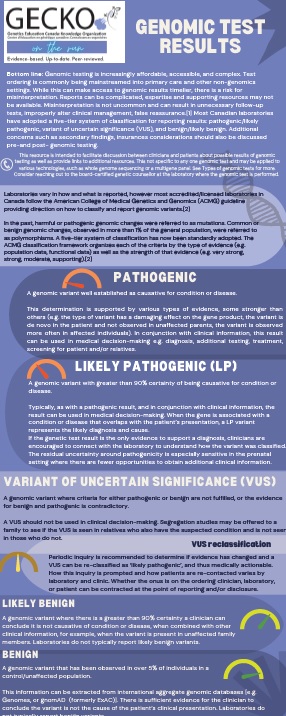
Bottom line: Genomic testing is increasingly affordable, accessible, and complex. Test ordering is commonly being mainstreamed into primary care and other non-genomics settings. While this can make access to genomic results timelier, there is a risk for misinterpretation. Reports can be complicated, expertise and supporting resources may not be available. Misinterpretation is not uncommon and can result in unnecessary follow-up tests, improperly alter clinical management, false reassurance.1 Most Canadian laboratories have adopted a five-tier system of classification for reporting results: pathogenic/likely pathogenic, variant of uncertain significance (VUS), and benign/likely benign. Additional concerns such as secondary findings, insurances considerations should also be discussed pre-and post- genomic testing.
Updated June 2025
Genomic test results
This resource is intended to facilitate discussion between clinicians and patients about possible results of genomic testing as well as provide links to additional resources. This not specific to any one genomic test and may be applied to various technologies, such as whole genome sequencing or a multigene panel. See Types of genomic tests for more. Consider reaching out to the board-certified genetic counsellor at the laboratory where the genomic test is performed.
Laboratories vary in how and what is reported, however most accredited/licensed laboratories in Canada follow the American College of Medical Genetics and Genomics (ACMG) guideline providing direction on how to classify and report genomic variants.2
In the past, harmful or pathogenic genomic changes were referred to as mutations. Common or benign genomic changes, observed in more than 1% of the general population, were referred to as polymorphisms. A five-tier system of classification has now been standardly adopted. Genomic variants are classified as: pathogenic, likely pathogenic, variant of uncertain significance, likely benign, or benign. The ACMG classification framework organizes each of the criteria by the type of evidence (e.g. population data, functional data) as well as the strength of that evidence (e.g. very strong, strong, moderate, supporting).2
Pathogenic (P)
A genomic variant well established as causative for condition or disease.
This determination is supported by various types of evidence, some stronger than others (e.g. the type of variant has a damaging effect on the gene product, the variant is de novo in the patient and not observed in unaffected parents, the variant is observed more often in affected individuals). In conjunction with clinical information, this result can be used in medical decision-making e.g. diagnosis, additional testing, treatment, screening for patient and/or relatives.
Likely pathogenic (LP)
A genomic variant with greater than 90% certainty of being causative for condition or disease.
Typically, as with a pathogenic result, and in conjunction with clinical information, the result can be used in medical decision-making. When the gene is associated with a condition or disease that overlaps with the patient’s presentation, a LP variant represents the likely diagnosis and cause.
If the genetic test result is the only evidence to support a diagnosis, clinicians are encouraged to connect with the laboratory to understand how the variant was classified. The residual uncertainty around pathogenicity is especially sensitive in the prenatal setting where there are fewer opportunities to obtain additional clinical information.
Variant of uncertain significance (VUS)
A genomic variant where criteria for either pathogenic or benign are not fulfilled, or the evidence for benign and pathogenic is contradictory.
A VUS should not be used in clinical decision-making. Segregation studies may be offered to a family to see if the VUS is seen in relatives who also have the suspected condition and is not seen in those who do not.
VUS reclassification
Periodic inquiry is recommended to determine if evidence has changed and a VUS can be re-classified as ‘likely pathogenic’, and thus medically actionable. How this inquiry is prompted and how patients are re-contacted varies by laboratory and clinic. Whether the onus is on the ordering clinician, laboratory, or patient can be contracted at the point of reporting and/or disclosure.
Likely benign
A genomic variant where there is a greater than 90% certainty a clinician can conclude it is not causative of condition or disease, when combined with other clinical information, for example, when the variant is present in unaffected family members. Laboratories do not typically report likely benign variants.
Benign
A genomic variant that has been observed in over 5% of individuals in a control/unaffected population.
This information can be extracted from international aggregate genomic databases [e.g. Genomes, or gnomAD (formerly ExAC)]. There is sufficient evidence for the clinician to conclude the variant is not the cause of the patient’s clinical presentation. Laboratories do not typically report benign variants.
Ordering clinician's role
The main purpose of genomic testing is to aid in diagnosis, support medical decision-making, clinical management, and individualized treatment. Laboratories will evaluate a variant and a gene in the context of the patient’s clinical presentation, family history, and previous laboratory tests – especially when attempting to resolve pathogenicity. To achieve optimal results, clinicians should provide complete and accurate clinical information about the patient. Clinicians may also be asked to obtain parental or other familial samples to assist in interpretation.
Considerations
Setting expectations: The implications of a positive result, where a pathogenic or likely pathogenic variant is identified, depend on the type of test. Testing types include:
- Predictive testing: performed on an unaffected individual, revealing if they will or will not develop a known familial condition e.g. Huntington disease.
- Predisposition testing: performed on an unaffected individual, where a positive result confers an increased risk to develop one or more conditions e.g. hereditary breast and ovarian cancer and an increased lifetime risk for certain cancers.
- Diagnostic testing: performed on a symptomatic individual who has a clinical presentation suggestive of an underlying genomic cause e.g. bilateral renal cysts possibly related to autosomal dominant polycystic kidney disease.
- Carrier status: often performed on individuals/couples who wish to assess the risk of having a child affected by an autosomal recessive condition. These results generally have no health implications for the individual identified as a carrier e.g. cystic fibrosis, Tay Sachs disease.
- Pharmacogenomic testing: Results provide information about how one’s genomic make-up affects response to medications. Results may be reported in response to pharmacogenomic testing or as Secondary/Incidental Findings (see below).
A true negative result is one where an individual is found not to carry a known familial pathogenic variant and so is not at risk for the familial condition. Their offspring would also not be at risk for the familial condition. Often this result is reassuring, but there may be feelings of survivor guilt. It is important to understand that this result is specific only to the familial condition tested for and does not eliminate any population risk or other familial risks.
A negative result, where no variants of clinical significance are found, can be reassuring depending on the diagnostic yield of the test ordered and the initial degree of clinical suspicion for a genomic etiology.
For example, the diagnostic yield of panel-based genomic testing for hypertrophic cardiomyopathy is estimated to be only about 30%.3 The greatest likelihood of finding a pathogenic/likely pathogenic variant is in those with a younger age of onset, a more ‘serious’ clinical presentation and a family history.3 Meaning, a negative cardiomyopathy gene panel result could be more reassuring in ruling out a genomic cause in a younger individual with a more serious clinical presentation and family history than in an individual who does not meet these criteria.
The best person in whom to begin genomic testing within a family is the person most likely to carry a pathogenic or likely pathogenic variant. Often, this is the youngest affected individual whose clinical presentation is most strongly associated with the diagnosis under investigation.
While negative results may be reassuring to some, they can be disappointing or frustrating to others who are looking for definitive answers. They may generate mixed emotions.
Variant of uncertain significance (VUS) is where a variant in a gene was identified, but its significance is not yet known. The laboratory cannot confidently determine if the gene variant identified is pathogenic or benign, as available evidence is insufficient or conflicting. A board-certified genetic counsellor or a geneticist can help to interpret the laboratory report. No changes to screening or medical management are indicated. Family members are typically not offered genetic testing for a VUS. Clinics and laboratories differ in their re-contact protocols, but generally a patient would be encouraged to re-contact their genetics provider in 2-5 years for updates on re-classification of the VUS they carry. Re-classification of a VUS could mean the variant is now determined to be pathogenic or benign.
Secondary/Incidental findings: Pathogenic and likely pathogenic variants may be identified in a gene unrelated to the clinical indication for testing. For example, where genomic testing is ordered to assist in diagnosis and treatment of a child with a neurodevelopmental disorder such as autism spectrum disorder, plus other features such as seizure, and/or regression of skills, testing could also uncover a pathogenic variant causing an adult-onset hereditary cancer condition. While these results are not medically actionable for the child, they would be for the adult relatives of that individual. In addition, they might inform future medical screening and surveillance of the child. The ACMG4 has published a guideline for clinical laboratories that includes a minimum list of genes to report where there is high actionability when a pathogenic or likely pathogenic variant is identified. There are currently 73 genes on the list and several on a ‘watchlist’.
In some testing circumstances, patients/parents of patients may have the option to opt in or out of receiving reports of secondary findings in additional genes. Genetic counselling should be offered in these circumstances. Genomic ADvISOR is a validated online decision aid to help patients make informed decisions about additional genomic information.
Insurance: There is protection for Canadians under the Genetic Non-Discrimination Act (GNA) passed in May 2017. Some key points of the law are that GNA prohibits:
- Discrimination based on genomic characteristics
- Providers of goods and services (including insurance) from:
- requesting or requiring a genomic test
- requesting or requiring the disclosure of genomic test results either past or future
- Federally regulated employers from using genomic test results in decisions about hiring, firing, job assignments, or promotions
Canadians considering genomic testing, particularly asymptomatic individuals or persons who have the potential to receive secondary findings, need not perceive discrimination as a negative consequence of such genomic testing. Note that many insurance companies do ask about conditions and diseases in relatives, and individuals may need to disclose a medical diagnosis e.g. cancer or Huntington disease, but not their genomic test results. A recent commentary in Canadian Family Physician discusses GNA and the implications for healthcare.5
Types of genomic tests
Karyotype: A high level genomic test that analyses the number and structure of an individual’s chromosomes. Used to identify extra or missing whole chromosomes or large pieces, as well as chromosomal rearrangements.
Microarray: A higher resolution (as compared to karyotype) genomic test to detect very small extra or missing pieces of genomic code (microdeletions and microduplications). These gains or losses are also called copy number variants (CNVs). DNA from two samples [case (patient) and control] are denatured (pulled apart), labelled, and hybridized (bound) to a small (micro) glass chip where thousands of short, single-stranded DNA sequences are arrayed. A computer scans the microchip and analyses the signal to determine if there are extra or missing sequences based on how the DNA binds to the slide.
Single gene test: Testing may be ordered when there is a clinical suspicion of a specific genetic condition known to be associated with a single gene (a monogenic disorder). Testing may include reading through all the coding regions of a gene (e.g. FBN1 gene for Marfan syndrome), counting the number of nucleotide repeats (e.g. CAG repeats in the HTT gene for Huntington disease) or targeted analysis to detect the presence or absence of specific genomic changes known to be associated with a condition (e.g. DF508 in the CFTR for cystic fibrosis).
Targeted variant analysis is a method of testing family members when a genomic variant has been identified in a relative. Family members are tested for the presence or absence of the specific genomic change. Documentation of the specific familial variant is important for testing.
Multigene panel: Genomic testing that reads through the coding regions of several genes at one time. Panels consist of multiple genes that are carefully selected based on the understanding that a genetic condition can be caused by a pathogenic variant in one of many genes (e.g. hereditary breast and ovarian cancer syndrome can be caused by pathogenic variants in the BRCA1 or BRCA2 gene, in addition to other genes). In addition to knowledge that a clinical presentation can be observed in several different genetic conditions, for example epilepsy can be present in Tuberous sclerosis complex (genes TSC1, TSC2), conditions resulting from an inborn error of metabolism (e.g. urea cycle disorders, genes CPS1, OTC, ASS1, ASL, ARG1, NAGS, SLC25A15, SLC25A13), classic Rett syndrome (gene MECP2), among many others.
Whole exome sequencing: Genomic testing that reads through each base of the coding regions (exons) of all the genes to identify variations in the sequences as compared to reference databases.
Whole genome sequencing: Genomic testing that reads through each base of both the coding (exons) and non-coding (introns) regions of all the genes to identify variations in the sequences as compared to reference databases.
This is not a comprehensive list but meant to highlight the most common Canadian clinical genomic tests.
Genomic testing sample requirements
Genomic testing is performed on DNA that can be extracted from various tissue sources. Most often clinical genomic testing is performed on a blood sample. The option of a buccal (cheek) swap or saliva sample is commonly available and can be particularly beneficial when there are barriers to obtaining a blood sample. Genomic testing may also be performed a skin biopsy, amniotic fluid or a placental biopsy.
References
[1] Donohue KE, Gooch C, Katz A, et al. Pitfalls and challenges in genetic test interpretation: An exploration of genetic professionals experience with interpretation of results. Clin Genet. 2021; 99(5):638-649. PMID: 33818754
[2] Richards S, Aziz N, Bale S, et al; ACMG Laboratory Quality Assurance Committee. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17(5):405-24; PMID: 25741868
[3] Hathaway J, Heliö K, Saarinen I, et al. Diagnostic yield of genetic testing in a heterogeneous cohort of 1376 HCM patients. BMC Cardiovasc Disord. 2021;21(1):126; PMID: 33673806
[4] Miller DT, Lee K, Chung WK, et al; ACMG Secondary Findings Working Group. ACMG SF v3.0 list for reporting of secondary findings in clinical exome and genome sequencing: a policy statement of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2021;23(8):1381-1390. Erratum in: Genet Med. 2021 Aug 3; PMID: 3401206
[5] Cowan JS, Kagedan BL, Graham GE, et al. Health care implications of the Genetic Non-Discrimination Act: Protection for Canadians' genetic information. Can Fam Physician. 2022;68(9):643-646. PMID: 36100377
Resources
- A one-page patient companion resource on genomic testing developed by Hannah Faghfoury, MD, FRCPC, FCCMG, geneticist at Mount Sinai Hospital and University Health Network [Accessed June 2025]
- Validated decision aid for individuals considering receipt of secondary findings following comprehensive genomic testing. Genomic ADvISOR [Accessed June 2025]
- A guide to genomic test results for non-genetics providers. Created by the Practitioner Education Working Group of the Clinical Sequencing Exploratory Research (CSER) Consortiumgenome.gov [Accessed June 2025]
- General genomics education at National Human Genome Research Institute [Accessed June 2025]