Prenatal Screening is an option available to everyone during pregnancy. You can decide whether or not you would like to have prenatal screening. The guide is meant to help people decide whether or not prenatal screening is right for them.
*New* Check out this 6-question preconception/prenatal family history screening tool
Table of Contents
- What are prenatal screening tests?
- The conditions for which prenatal screening is used
- Are prenatal screening tests right for me?
- I have decided
- Nuchal translucency
- Table 1. Prenatal screening tests available and how they compare
- What is non-invasive prenatal testing by cell-free DNA?
- What are the benefits of NIPT/cfDNA screening?
- What are the limitations of NIPT/cfDNA screening?
- Who should have NIPT/cfDNA screening?
- Who offers NIPT/cfDNA screening?
- Table 2. Non-Invasive Prenatal Testing (NIPT) in Canada. Not every test is available everywhere. Last updated November 2023.
- What do my screening results mean?
- What are the next steps if my prenatal screening test is POSITIVE?
- Diagnostic procedures
- A word about unexpected news
- A prenatal screening process map
- Online resources
- Acknowledgements
- Additional resources
In Canada, about 1 in 25 (4%) babies is born with a difference or variation, called a congenital anomaly, which may require medical or surgical intervention. The most common variations are structural heart defects, cleft lip and/or palate or a pattern of variations such as Down syndrome. Some risk factors, like family history or the pregnant person/egg donor’s age, can increase the chance that a person will have a baby with an anomaly. If you have any concerns about your family history, for example you have a genetic condition, there are close relatives with intellectual disability or who were born with one or more anomalies, young children or babies that passed away unexpectedly, be sure to discuss that with your health care practitioner.
Through available prenatal screening and detailed second trimester ultrasound, the chance to have a baby with some specific genetic conditions and anomalies can be more precisely determined. Prenatal screening is about risk assessment
What are prenatal screening tests?

Prenatal screening is available to people expecting a baby.
Test options vary in each region.
These are blood tests, sometimes accompanied by an ultrasound, that are performed early in pregnancy.
Prenatal screening determines your chance of having a baby with Down syndrome, trisomy 18 or an open neural tube defect. Prenatal screening can sometimes determine the chance of other genetic conditions and anomalies.
Many people expecting a baby have a difficult time deciding whether or not to have a prenatal screening test. Some people find it helpful to read this entire guide first, before making a decision.
The conditions for which prenatal screening is used
Down syndrome

People with Down syndrome are individuals who are just as unique and highly variable as anyone else. An individual with Down syndrome has an extra copy of chromosome 21 (trisomy 21). This usually causes mild to moderate intellectual disability, which means that adults will typically function at the level of an 8-10 year old. An individual with Down syndrome is expected to learn to read and write and to be physically active, however major developmental milestones will be delayed. Individuals with Down syndrome have a greater possibility of health conditions than the average person, such as heart, stomach, bowel, thyroid, vision and hearing problems. Treatment is available for many of these conditions. There is no way to predict how serious or mild these differences will be. The average life expectancy for a person with Down syndrome is now about 60 years old. In general, about one in 781 babies born has Down syndrome. The chance of having a child with Down syndrome increases with the pregnant person/egg donor’s (in the case of a donated egg) age (See Table 3 in Additional Resources). For more information on Down syndrome, visit the Canadian Down Syndrome Society website.
Trisomy 18
Babies with trisomy 18 have an extra chromosome 18. Every individual with trisomy 18 is different, however serious intellectual disabilities and congenital anomalies that may affect many organ systems (e.g. heart, kidneys) are expected. Many pregnancies with trisomy 18 will miscarry. Most babies born with trisomy 18 do not survive past the first few months of life. About 10% of infants will survive up to 5 years of age, or occasionally longer. Long-term survivors are described as socially interactive with significant physical and intellectual disabilities (e.g. having few words). In general, about one in 6,000 babies born has trisomy 18. The chance of having a child with trisomy 18 increases with the pregnant person/egg donor’s age. For more on trisomy 18, visit The Trisomy 18 Foundation website.
Open Neural Tube Defects
The neural tube is a structure in the early development of the central nervous system (the spinal cord and the brain). This structure is completely formed by about 6 weeks of pregnancy. Incomplete or failed formation of the neural tube leads to congenital anomalies of the brain or spinal cord and nerves. The effects of a neural tube defect are extremely varied and depend on the location and size of the defect. Open neural tube defects are the most common and serious. The neural tube defect is closed if the defect is covered by skin and the neural tissue is not exposed to amniotic fluid. A neural tube defect involving the spinal cord is called spina bifida. Spina bifida causes physical disabilities such as difficulty walking, and controlling the bladder and/or bowel. People with spina bifida may also have intellectual disabilities. Treatment can help with many of the physical disabilities. A neural tube defect involving the brain is called anencephaly. A baby with anencephaly will be stillborn or die shortly after birth. In Canada, the chance of having a baby with an open neural tube defect is about one in 1000 live births. The chance does not increase with the pregnant person/egg donor’s age. The chance does decrease when a prenatal vitamin with folic acid is taken. For more on spina bifida, see the Spina Bifida & Hydrocephalus Association of Ontario website. Talk to your health care provider about folic acid and prenatal vitamins.
Additional conditions which may be screened for by prenatal screening:
Trisomy 13 (Patau syndrome)
Babies with trisomy 13 have an extra chromosome 13. In general between 1/8,000 and 1/15,000 of babies born has trisomy 13. The chance of having a child with trisomy 13 increases with a pregnant person/egg donor’s age. Every individual with trisomy 13 is different; however each individual is expected to have both serious intellectual disabilities and congenital anomalies, including differences of the brain, heart, eyes and face. Most pregnancies with trisomy 13 will miscarry. About 5-10% of infants will survive the first year of life. There are some individuals who have lived to adulthood. For information on trisomy 13, visit Support Organization for Trisomy 18, 13 and Related Disorders (SOFT) website www.trisomy.org. See Additional Resources for more information about genetics.
Sex chromosome differences
Typically, each mature human cell contains 23 chromosome pairs (46 chromosomes in total). One of these chromosome pairs, the 23rd pair, is the sex chromosomes. A female cell will usually have two X chromosomes and a male cell will have one X chromosome and one Y chromosome. Some prenatal screening and diagnostic testing can identify extra or missing X and/or Y chromosomes. There are several conditions with sex chromosome differences. Generally, these types of genetic differences are quite common occurring in about 1 in 500 individuals. Expected features are variable and depend on which chromosome is extra or missing. Some features maybe as mild as tall or short size. There may be differences in development such as delayed speech or learning differences. There may be associated health issues involving puberty or the heart. Visit The Association for X and Y Chromosome Variations (AXYS) or the Turner Syndrome Society of Canada for more.

Remember…
You might decide to have prenatal screening because you want to know the chance that your baby has one of the conditions previously described. Prenatal screening uses the age of the pregnant person/egg donor, blood test(s) and/or ultrasound of the baby to determine a more accurate chance.
Are prenatal screening tests right for me?
It is your choice whether or not to have a prenatal screening test. There is not a right or wrong choice.
To help your decision-making, here are some questions people may ask themselves and discuss with a partner, health care practitioner, spiritual leader, family or friends.
- Do I want to know the chance of my baby having Down syndrome, trisomy 18 or open neural tube defect?
- What would I do with this information?
Consider…
- What could you do with this information:
- Pregnancy management: If you are found to be at increased risk for one of these conditions, your health care practitioner may suggest additional tests (e.g. diagnostic testing, more ultrasounds) and/or suggest changes to how your pregnancy is managed or the way your baby is delivered.
- Reproductive choice: If I have a child with intellectual and/or physical disabilities, how might this affect my life, my other children, and my relationship with my partner and my extended family? Some people expecting a baby have screening because they would like the information before birth to help with decision-making in the pregnancy. If their baby was found to have one of these conditions they would:
- prepare for a child with special needs (See point 5 for more)
- consider giving the baby up for adoption
- consider ending the pregnancy
- Some people expecting a baby choose to not have screening because they would not:
- have a diagnostic test under any circumstance because of the small risk of miscarriage
- change the course of their pregnancy by choosing to end the pregnancy
Remember that most babies are born without an anomaly, however 1 in 25 babies in Canada is born with a difference at birth requiring medical intervention (congenital anomaly). Prenatal screening does not screen for all possible anomalies. There is no cure for Down syndrome, trisomy 18 or open neural tube defect.
- How will this information affect my feelings throughout the pregnancy?
A low risk (screen negative) result is the most common outcome and those expectant individuals are likely to feel reassured
Consider…
how would I feel if I received an increased chance (screen positive) for one of these conditions? Many people expecting a baby experience anxiety and worry when their test results say that the chance of having a baby with one of these conditions is higher than expected.
- If your screening test result says there is an increased chance (screen positive) your baby has Down syndrome, trisomy 18 or open neural tube defect, you will need to decide if you want diagnostic testing. A screening test can only tell you the chance (probability) that your baby has one of these conditions. A diagnostic test can tell you for sure whether or not your baby does have the condition. Prenatal diagnostic testing for Down syndrome or trisomy 18 consists of amniocentesis or chorionic villus sampling (CVS). In the case of open neural tube defects, diagnostic testing will include a detailed ultrasound, amniocentesis or other investigation.
Would I pursue diagnostic testing in the event of a screen positive result?
Consider…
- Diagnostic testing will tell you if your baby has or does not have one of these conditions, but with amniocentesis and chorionic villus sampling (CVS) procedures there is a small chance of miscarriage (less than 1%).
- Would I be willing to take that risk to have this information?
- Diagnostic testing can also detect conditions for which you were not known to be at increased risk, such as another chromosome difference.
- Would I want this additional information about my baby?
- If Diagnostic testing confirms a baby has the condition, people expecting a baby need to decide if they want to continue the pregnancy or if they will end the pregnancy.
- If more testing shows that my baby has a condition for sure, what will I do with the information? (See points 1, 2 and 5 for more)
- 5. If you know that you would not end a pregnancy for any reason, prenatal screening may still be an option for you. With a prenatal diagnosis you can: plan for the birth of your child; find out from others what it is like to raise a child with this condition; learn about resources available in your community; meet with various health care teams who may be involved with your child’s care; or look into adoption.
Consider…
- Before the baby is born, to know for sure if a baby has one of these conditions, a diagnostic test like amniocentesis or chorionic villus sampling (CVS) is needed. Remember diagnostic tests are invasive and have a small chance of causing miscarriage
- Diagnostic testing for a chromosome difference can be performed on a blood sample once a baby is born. This is a non-invasive option for people expecting a baby who would not change the course of their pregnancy based on such a diagnosis
- Would this information be helpful to me before the birth or can I wait until my baby is born?
I have decided…
A. I do not want to have prenatal screening, now what?
Your health care practitioner will follow you as in any other pregnancy and make sure that both you and your baby are in the best possible health. Where available, you may be offered an ultrasound in the late first trimester (around 11-14 weeks gestation) for more accurate dating of your pregnancy, determination of twins, and early detection of major congenital anomalies. You may be offered an ultrasound in the second trimester at around 18 20 weeks gestation to look at the baby’s growth and anatomy.
B. I do not want to have prenatal screening but rather diagnostic testing, now what?
Your access to diagnostic testing will vary depending on where you live. If you, or in the case of a donor, the egg, will be 40 years or older at the time of birth you will likely have the option to choose diagnostic testing without prenatal screening. Talk to your health care practitioner about next steps. See diagnostic testing for more, and for more on available genetic tests see Additional Resources.
C. I do want to have prenatal screening, now what?
Once you have decided to proceed with prenatal screening, the next step is for you and your health care practitioner to choose which testing option is right for you. The following two tables compare available screening tests. Some factors that affect which prenatal screening tests you can choose from are:
- — Where you live
- Screening choices vary according to where you live. Your health care practitioner will discuss what is available.
- — How far along you are in the pregnancy
- Accurate dating of your pregnancy, determined by a first trimester ultrasound, is important for accurate screening results. Dating based on last menstrual period (LMP) is not ideal, but if a first trimester ultrasound is not available this dating can be used.
- If the first prenatal visit with your health care practitioner is before 14 weeks (3 1/2 months) of pregnancy, options that may be presented to you include:
- Enhanced First Trimester Screening (eFTS) and/or Non-Invasive Prenatal Testing (NIPT)
- If the first prenatal visit with your health care practitioner is after 14 weeks (3-1/2 months) and before 21 weeks (~5 months) of pregnancy, options that may be presented to you include:
- Multiple Marker Screening (MMS), Second Trimester Screening (STS) and/or Non-Invasive Prenatal Testing (NIPT)
- — The age of the pregnant person (or the egg in the case of a donated egg) when the baby is born
- If the pregnant person will be 40 years of age or older at the time of birth, prenatal testing options include all screening tests above, possibly, in addition to the option of diagnostic testing.
- If the pregnant person/egg donor will be 39 years of age or younger at the time of birth, prenatal options include all of the screening tests above. NIPT is also available, but may require out of pocket payment
- — Whether or not twins or higher order multiples (e.g. triplets) are present
- Not all screening tests perform well when there is more than one baby
- Non-Invasive Prenatal Testing (NIPT) and/or diagnostic testing may be offered
- Not all screening tests perform well when there is more than one baby
Nuchal translucency
In addition to blood work, many screening tests also include an ultrasound measurement called the nuchal translucency (NT). What is the NT measurement?

The NT is a fluid filled space at the back of every baby’s neck (see image left)
- A larger NT measurement is associated with an increased chance for chromosome conditions like Down syndrome and some other genetic and non-genetic issues like congenital heart defect
- An ultrasound to measure NT is performed between 11 and 14 weeks of pregnancy and should be done at a certified ultrasound site. Your health care practitioner will tell you where an NT ultrasound can be obtained.
- An NT measurement of 3.5mm or bigger is considered significant and would be a screen positive. A referral for genetic counselling will likely be offered.
Table 1 has an overview of the prenatal screening tests available in Ontario and how they compare to each other. Not all test options are available in all areas.
Enhanced First Trimester Screening (eFTS) is the most commonly offered prenatal screening test. It screens for Down syndrome and trisomy 18. Results from eFTS are available early in pregnancy, allowing people time for decision making and access to additional services.
A person who presents to their first prenatal visit at a later gestational age (after 14 weeks) may be offered Multiple Marker Screening (MMS)/Second Trimester Screening (STS).
An ultrasound is recommended for all pregnant individuals at about 18 20 weeks of pregnancy to look at the baby’s growth and anatomy, regardless of prenatal screening results. While most babies are born without anomalies, 1 in 25 babies in Canada will be born with a difference that may require medical intervention. It is important to remember that no test can detect every type of anomaly.
If you are expecting twins, prenatal screening is available but in general is not as accurate as for pregnancies with one baby. Also, not all screening options will be available for a twin pregnancy. Talk to your health care provider for more about screening in a twin pregnancy.
Remember…
Your health care practitioner will help you choose the right prenatal screening test for you. Factors that affect what is available are: where you live, gestational age of the pregnancy at the time of the first prenatal visit, pregnant person/egg donor’s age at the time of birth, whether one or more babies are present.
The nuchal translucency (NT) can only be measured between 11 and 14 weeks of pregnancy at a certified ultrasound centre. This is a normal fluid filled space in every baby. You will likely be offered a referral to your local genetics centre if the NT measurement is greater than 3.5mm.
Table 1. Prenatal screening tests available and how they compare.
Enhanced First Trimester Screening (eFTS)Non-Invasive Prenatal Testing (NIPT)/cfDNA screeningMultiple Marker Screening (MMS)
| Components of test All screens use the pregnant person/egg donor’s age in risk assessments u/s = ultrasound NT = nuchal translucency |
|
One blood test for cell-free (cf) DNA | One blood test for 3-4 pregnancy related hormones |
| Gestational age at first trimester blood test |
11 – 13 weeks |
Recommended after 10 weeks | Not applicable |
| Gestational age at the NT ultrasound |
11 – 13 weeks |
Not applicable | Not applicable |
| Gestational age at second trimester blood test | Not applicable | Not applicable |
15 – 20 weeks |
| Detection rate (these are approximate and depend upon the actual test/laboratory) |
Meaning, how many pregnancies where the baby really does have Down syndrome will be flagged as increased risk this test? | ||
| 85-90% | 99% | 80% | |
| False positive rate (these are approximate and depend upon the actual test/laboratory) |
Meaning, how many pregnancies will this test flag as increased risk BUT the baby does NOT really have Down syndrome? | ||
| About 3-6% | Less than 0.1% | About 5% | |
| Conditions screened for |
|
|
|
Non invasive prenatal testing by cell-free DNA: the latest in prenatal screening
What is non-invasive prenatal testing by cell-free DNA?
Non-Invasive Prenatal Testing (NIPT) is a screening test to estimate the chance that the unborn baby has Down syndrome or another chromosome condition (trisomy 18, trisomy 13 or an extra or missing sex chromosome). Normally genetic information (DNA) is contained within a cell (see the Additional Resources for an introduction to genetics). When a cell dies it releases its contents into the blood stream and the DNA is broken up into tiny pieces. This DNA is called cell-free DNA (cfDNA).
NIPT is also known as cfDNA screening. NIPT/cfDNA screening detects, reads and counts cfDNA in a pregnant person’s blood stream. Although this cfDNA is not directly from the baby, it is from the placenta and usually does represent the genetic profile of the baby.
What are the benefits of NIPT/cfDNA screening?
- Accuracy: NIPT/cfDNA screening is more accurate than conventional prenatal screening tests, detecting more than 99% of pregnancies where the baby has Down syndrome (versus 75-90% by other screening methods). See Table 1 for more on conventional prenatal screening.
- Fewer invasive (diagnostic) procedures: As the performance of NIPT/cfDNA is better than conventional prenatal screening, fewer pregnancies will be flagged as increased risk (screen positive) and go onto have diagnostic testing associated with small risk of miscarriage
- Timing: The result from NIPT/cfDNA screening is available earlier than conventional prenatal screening. NIPT/cfDNA screening is just one blood test. Current Society of Obstetricians and Gynaecologists of Canada (SOGC) guidelines recommend that NIPT/cfDNA screening is performed after 10 weeks of gestation. Results are available about 1-2 weeks after testing. Having screening results earlier in pregnancy allows people expecting a baby more time for decision-making and potentially offers them more options.
Who should have NIPT/cfDNA screening?
NIPT/cfDNA screening is available to all pregnant people.
NIPT/cfDNA screening can be used as a second screen (i.e. after receiving a positive Enhanced First Trimester Screening result or if specific ultrasound differences have been found) or as a first screening test (e.g. before any other screening).
When there is an increased chance for a baby to have a chromosome condition, recommendations are that screening by NIPT/cfDNA be considered. In general, a pregnancy is considered to be at increased risk for a chromosome condition when:
- The pregnant person is 40 years of age or older at the time of estimated date of birth
- There are twins present
- There is a screen positive result by conventional prenatal screening
- The nuchal translucency (NT) measurement is 3.5mm or greater on first trimester ultrasound
- There is a history of a previous pregnancy or child with a chromosome condition (e.g. Down syndrome, trisomy 18 or 13)
- There are ultrasound findings highly suggestive of a chromosome condition
- There is a risk, based on family history, of carrying a male fetus with an X-linked condition such as hemophilia or Duchene muscular dystrophy
- NIPT/cfDNA screening could be used for sex determination
Who should have NIPT/cfDNA screening?
NIPT/cfDNA is typically offered by the most responsible prenatal care practitioner. This may be your family physician, nurse practitioner, obstetrician or genetic counsellor. NIPT/cfDNA is available in every province and territory. Public healthcare funding may be available if certain criteria are met. You can find links to your provincial prenatal screening program here and whether NIPT/cfDNA is funded in your area here.
Several companies offer NIPT/cfDNA through provincial programs and as private pay testing. The cost of NIPT/cfDNA varies but in general is about 100-400$. GECKO does not endorse one company over another. Your local genetics centre may provide information about the locally available test.
Several companies offer NIPT/cfDNA through provincial programs and as private pay testing. The cost of NIPT/cfDNA varies but in general is about 100-400$. GECKO does not endorse one company over another. Your local genetics centre may provide information about the locally available test.
Table 2 below has some information about NIPT/cfDNA testing companies available in Canada. The technology each company uses to calculate the risk of a chromosome condition is different, but the accuracy of the tests is comparable. If you choose to have NIPT/cfDNA, the company you and your health care practitioner choose may vary depending on factors listed in Table 2.
Table 2. Non-Invasive Prenatal Testing (NIPT) in Canada. Not every test is available everywhere.
HarmonyTM by AriosaPanoramaTM by NateraNIPS by Invitae
| Where is my blood drawn for this test? | DynaCare | LifeLabs Genetics | Mobile phlebotomist |
| How early can I have this test? | 10 weeks gestation | 9 weeks gestation* | 10 weeks gestation |
| When would results be available? | 10 business days | 7-10 calendar days | 3-10 calendar days |
|
Will this test work if this pregnancy:
|
Yes | Yes | |
|
Yes | Yes | |
|
Yes | Yes | |
|
Yes | Yes | |
| What proportion of the pregnancies where the baby does have Down syndrome will be detected? (Detection rate) | >99% | >99% | >99% (as per company) |
| What proportion of the pregnancies where the baby does not have Down syndrome will be falsely called high risk? (False positive rate) | Less than 1 in 1,000 (0.1%) | Less than 1 in 1,000 (0.1%) | |
| Is genetic counselling available through the company?+ | Yes | Yes | Yes |
| Cost** | $495 | $550 |
*The Society of Obstetricians and Gynaecologists of Canada guidelines recommend that NIPT/cfDNA screening is performed after 10 weeks of gestation because, prior to that time, there is an increased chance that the test will not give a result and will need to be repeated.
+Make sure the individual providing genetic counselling is a Canadian or American board-certified genetic counsellor to ensure that individual has met standards for providing competent genetic counselling care.
** Cost varies based on test options e.g. NIPT screening for chromosomal abnormalities alone or NIPT screening for chromosomal abnormalities and microdeletion syndromes.
Harmony and Panorama have agreements with the Ministry of Health and Long-term Care in Ontario [other provinces may have agreements as well]. They provide test performance data to the Better Outcomes Registry & Network allowing for quality assurance insight. Invitae does not and testing is performed outside of Canada.
What about the other genetic conditions screened for by NIPT/cfDNA screening?
You may have read that the NIPT/cfDNA screening can suggest other genetic conditions, such as microdeletion and microduplication syndromes. These are rare genetic conditions, occurring in about 1 in 5,000 to 1 in 50,000 pregnancies. They are caused by very tiny extra or missing pieces of chromosomes.
Most of these conditions occur by chance, meaning that they tend to not run in families and can occur out of the blue. The risk of these conditions is not associated with the pregnant person/egg donor’s age, as it is for Down syndrome and trisomy 18 (conditions caused by extra whole chromosomes).
The addition of these rare conditions to NIPT/cfDNA screening increases the false positive rate. This means that more people would receive a positive (high risk) screen result even though the baby does not actually have the condition. This would result in more people having diagnostic tests, with associated risk of miscarriage. Current recommendations do not support the routine inclusion of screening for microdeletion and microduplication syndromes in NIPT/cfDNA screening.
Remember…
Non-Invasive Prenatal Testing (NIPT), also known as cfDNA screening, is a test to estimate the chance that the baby a person is carrying has Down syndrome and other specific genetic conditions.
NIPT/cfDNA screening is available to all pregnant people. Some provincial prenatal screening programs will pay for NIPT/cfDNA screening when certain increased risk criteria are met. Where provincial funding is not available, people can self-pay for NIPT/cfDNA screening. Prices vary by company, the average cost being around $500.
Benefits: NIPT/cfDNA screening is much better at detecting Down syndrome and other specific genetic conditions than conventional prenatal screening (e.g. Enhanced First Trimester Screening). NIPT/cfDNA screening has a lower false positive rate than conventional prenatal screening. Higher detection and lower false positive rates mean that fewer people will need to have follow-up invasive testing which is associated with a small risk of pregnancy loss.
Limitations: NIPT/cfDNA screening is not diagnostic, meaning that it cannot tell with certainty whether or not the baby a person is carrying has Down syndrome or another genetic condition. A person who receives a high risk or positive NIPT/cfDNA screening result will be offered diagnostic testing by amniocentesis or chorionic villus sampling to confirm or rule out the diagnosis. NIPT/cfDNA screening cannot detect all possible genetic conditions. There is no screening or diagnostic test which can guarantee a baby that does not any birth difference or any genetic condition. A person who receives a low risk NIPT/cfDNA screening result may still be offered additional counselling or testing depending on why they were originally offered NIPT/cfDNA screening.
What do my screening results mean?
A: Screening results using Enhanced First Trimester Screening as an example:
Enhanced First Trimester Screening (eFTS) calculates the chance that the baby has Down syndrome or trisomy 18. It does not screen for open neural tube defects or any other condition. eFTS uses the age of the pregnant person/egg donor at the time of delivery, the size of the nuchal translucency (NT) on a first trimester ultrasound, and the levels of certain hormones in the pregnant person’s blood that are being produced by the current pregnancy. A risk is then calculated estimating the chance that the baby has either condition. Generally, for eFTS, a risk greater than 1/350 (~0.3%) is considered screen positive and any risk lower than this is a screen negative. For more on eFTS see Section I have decided. I do want to have prenatal screening, now what?.
What if my eFTS result is a screen NEGATIVE?
This is reassuring. This means that the chance that your baby has Down syndrome or trisomy 18 is LOWER than the screening cut-off (for example less than 0.3% or 1/350). Note that the screening cut-off may vary by laboratory and condition.
What do I do next?
Remember eFTS is only intended to screen for Down syndrome and trisomy 18. eFTS is not intended to screen for any other conditions. An ultrasound is recommended for all individuals expecting a baby at about 18 20 weeks of pregnancy to look at the baby’s growth and development, regardless of prenatal screening results. While most babies are born without a birth difference, 1 in 25 babies in Canada will be born with a difference that may require medical or surgical intervention. It is important to remember that no test can detect every type of congenital anomaly (birth difference).
What if my eFTS result is a screen POSITIVE?
This means that the chance of your baby having Down syndrome or trisomy 18 is HIGHER than the screening cut- off (for example greater than 0.3% or 1/350). This result does not necessarily mean that your baby has one of these genetic conditions. Remember that most babies are born without anomalies.
A nuchal translucency (NT) measurement greater than 3.5mm is an automatic screen positive for Down syndrome and certain other conditions and should prompt a referral for genetic counselling.
Is an eFTS screen POSITIVE result accurate?
eFTS will identify most (about 85- 90%) pregnancies where the baby has Down syndrome.
eFTS does not perform as well when detecting trisomy 18, however it will identify most pregnancies with trisomy 18.
While eFTS is excellent at identifying most pregnancies where the baby has Down syndrome or trisomy 18, most screen positive results turn out to be false. This is called a FALSE POSITIVE and is identified either by diagnostic testing or by the birth of a baby who does not have the condition.
eFTS does not screen for open neural tube defects.
eFTS is not meant to screen for any other disorders.
What do I do next?
See the section What are the next steps if my prenatal screening test is POSITIVE?
B: Screening results using non-invasive prenatal testing (NIPT) as an example:
NIPT/cfDNA screening is a newer and more accurate way to screen for Down syndrome, trisomy 18, trisomy 13 and sex chromosome differences in a pregnancy. NIPT examines DNA in the pregnant person’s blood that comes from the pregnancy.
What if my NIPT/cfDNA screening result is NEGATIVE?
This is very reassuring. Generally, an NIPT/cfDNA screen NEGATIVE result is reported as LOW RISK (less than 1 in 10,000 chance). The chance that your baby has Down syndrome, trisomy 18, trisomy 13 or a sex chromosome difference is LOWER than that. NOTE: In twin pregnancies, it is not possible to screen for sex chromosome differences.
What do I do next?
Remember NIPT/cfDNA screening is only intended to screen for Down syndrome, trisomy 18, trisomy 13 and sex chromosome differences. You may be offered a late first trimester ultrasound (11-14weeks). Additionally, an ultrasound is recommended for all individuals expecting a baby at about 18 20 weeks of pregnancy to look at the baby’s growth and anatomy, regardless of prenatal screening results. While most babies are born without a birth difference, 1 in 25 babies in Canada will be born with a difference that may require medical or surgical intervention. It is important to remember that no test can detect every type of anomaly.
If you had NIPT/cfDNA screening because a first trimester ultrasound found the nuchal translucency measurement was 3.5mm or greater, a referral for genetic and/or maternal fetal medicine consultation is still recommended. Additional testing and/or follow-up may still be offered for example a special ultrasound of the baby’s heart, or other types of genetic testing.
What if the risk number reported is not less than 1 in 10,000?
If you received a risk result other than less than 1 in 10,000 (e.g. another low risk value or a borderline risk) you should discuss this result with your health care practitioner or genetic counsellor. This test is still relatively new and additional follow up testing and/or counselling may be needed.
What if my NIPT/cfDNA screening test fails?
Occasionally NIPT/cfDNA screening may fail and no result is reported. There are various reasons why a test may fail, What are the limitations of NIPT/cfDNA screening? for more. In this event, you may be asked for a new blood sample. Most of the time a result will be available after this second try. This can delay results and so it would be important to consider if the result would be received in a timely manner for decision-making. If the second try is also unsuccessful you may be offered genetic counselling to discuss this and additional testing options.
What if my NIPT/cfDNA screening result is POSITIVE?
An NIPT/cfDNA screen POSITIVE result is generally reported as HIGH RISK (greater than 99% chance). NIPT/cfDNA screening has a very low false positive rate meaning that further testing is expected to confirm the diagnosis and most screen positives will be true positives.
However, NIPT/cfDNA screening is not a diagnostic test and there is still a small chance that a high-risk result is false. In the event of a screen positive NIPT/cfDNA result, diagnostic testing is recommended prior to any permanent action (e.g. choosing to end the pregnancy). Information gained from diagnostic testing is also helpful for future counselling about recurrence risks in future pregnancies. If people expecting a baby would continue the pregnancy regardless of diagnostic results, chromosomal testing can be arranged after the baby is born.
Is an NIPT/cfDNA screen POSITIVE result accurate?
NIPT/cfDNA screening will identify about 99% of pregnancies (99 out of 100) where the baby has Down syndrome. N I PT/cfDNA screening does not perform as well when detecting trisomy 18 and even less so when detecting trisomy 13 and sex chromosome differences, however it is still considered a superior screen to traditional prenatal screening (Table 1) for these conditions.
What do I do next?
See the next section What are the next steps if my prenatal screening test is POSITIVE?
What are the next steps if my prenatal screening test is POSITIVE?
If your prenatal screening result is reported as positive or high risk for a chromosome condition (i.e. Down syndrome, trisomy 18), you are likely to be offered an appointment with a genetic counsellor. There you will discuss what this result means and your options, including no further testing, or a diagnostic test such as amniocentesis or chorionic villus sampling (CVS). Genetic counsellors can help you understand your options and make the decision that is right for you. They will support your decision no matter what you decide.
If your result is screen positive for a neural tube defect, you may have the option of a detailed ultrasound at 18 to 20 weeks instead of amniocentesis. This will vary depending on where you live.
There are many factors that influence peoples’ decisions to choose one option over another following a positive prenatal screening result. Some important considerations are:
- What information from diagnostic testing may be used for
- reassurance
- reproductive planning e.g. planning for a future with a child with special needs, or adoption or choosing to end the pregnancy
- see Are prenatal tests right for me? for more
- How far along the pregnancy is
- time is an important consideration in pregnancy decisions
- in Canada, while there are no legal restrictions on ending a pregnancy by medical termination, the availability is different in each city. Typically, before 22 weeks of pregnancy, medical termination can be accessed. After this, special arrangements may need to be made. Your health care practitioners and/or genetic counsellor will be able to help you learn what is available to you.
- The risk reported by the screening test
- a screen positive risk score of 1/200 (0.5%) versus a screen positive risk score of 1/2 (50%) may weigh differently on peoples’ decisions

When deciding about whether or not you wish to proceed with diagnostic testing you should consider what you might do in the event that the results say your baby does have the condition. You do not have to decide before testing what you would do in the event a diagnosis is confirmed; however preparing yourself to make such a decision can be important. Your health care practitioner will also discuss your choices with you. You may want to discuss this with your partner, friends, family, spiritual leader or other supports.
Consider…
Based on the risk number you have been given, whether it is a 1 in 10 (10%) or a 1 in 100 (1%), can you continue your pregnancy with that level of uncertainty or do you need to know for sure?
What if diagnostic testing has been offered to me?
Diagnostic procedures
Where screening tests calculate a risk (what is the chance), a diagnostic test/procedure will rule in or rule out for sure whether or not a baby has one of the conditions. There are two common diagnostic tests that are offered: chorionic villus sampling (CVS) and amniocentesis. Whereas prenatal screening tests are considered non-invasive as they pose no risk to a pregnancy, diagnostic tests are considered invasive because they are associated with a small procedural risk – an increased chance to lose the pregnancy (miscarriage).
Chorionic villus sampling (CVS)
What is chorionic villus sampling?
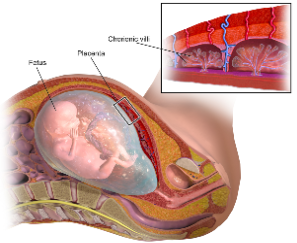
Chorionic villus sampling (CVS) is a procedure where a small piece of the placenta is taken and tested. Chorionic villi (see image on the right) attach the placenta to the uterus wall. The placenta is made from the fertilized egg and is expected to have the same genetic information as the baby. CVS is not available in all regions. Talk to your health care practitioner to see if this is an option for you. CVS cannot detect open neural tube defects.
When is a CVS carried out?
CVS is usually performed between 11 and 13 weeks of pregnancy.
What is the risk associated with CVS?
Both CVS and amniocentesis have been associated with a slightly increased chance of losing the baby following the procedure (miscarriage). The chance of miscarriage after a CVS or an amniocentesis is 0.5 to 1% (about 1 in 100 or less).
Both CVS and amniocentesis have been associated with a slightly increased chance of losing the baby following the procedure (miscarriage). The chance of miscarriage after a CVS or an amniocentesis is 0.5 to 1% (about 1 in 100 or less).
What should I expect at my CVS appointment?
CVS is an outpatient procedure, meaning that you will not need to stay overnight in the hospital. You will be told to have a full bladder. There are two methods to collect a sample from the placenta; either through the vagina or the abdomen. Both methods use ultrasound as a guide the entire time.
Through the vagina, using ultrasound, a speculum is inserted (just like a Pap test). Then a very thin, plastic tube is inserted up the vagina and into the cervix. The tube is guided up to the placenta and a small sample is removed.
To collect a sample through the abdomen, a thin needle is inserted through the abdominal wall, using ultrasound to guide the needle tip to the placenta.
Will it be painful?
Most people describe the procedure as uncomfortable rather than painful. In general, no medication or anesthetic is given. Through the vagina, the discomfort is similar to that with a Pap test. Through the abdomen, the pain from the needle is similar to having a blood sample drawn. The needle is a bit thicker and a numbing cream may be applied to the skin prior to the procedure. You can expect to experience some uterine cramping during the procedure.
Amniocentesis
What is amniocentesis?
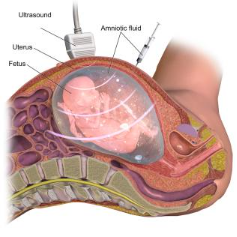
Amniocentesis is a procedure where a small sample of amniotic fluid (the fluid that surrounds the baby) is removed and tested. Usually only about 1-2 tablespoons are taken. Amniotic fluid contains fetal cells: skin cells and others cells that are naturally shed by the baby.
When is an amniocentesis carried out?
The ideal timing is between 15 and 18 weeks to allow opportunity for the procedure, results and decision making. An amniocentesis can, however, be performed any time after 15 weeks.
What is the risk associated with amniocentesis?
Both CVS and amniocentesis have been associated with a slightly increased chance of losing the baby following the procedure (miscarriage). The chance of miscarriage after a CVS or an amniocentesis is 0.5 to 1% (about 1 in 100 or less).
What should I expect at my amniocentesis appointment?
Amniocentesis is an outpatient procedure, meaning that you will not need to stay overnight in the hospital. You may be told to have a full bladder, but this will likely depend on how far along in pregnancy you are.
To collect a sample of amniotic fluid, using ultrasound guidance the entire time, a thin needle is inserted through the abdominal wall into a pocket of fluid (not near the baby) and fluid is extracted.
Will it be painful?
Most people describe the procedure as uncomfortable rather than painful. In general, no medication or anesthetic is given. The pain from the needle is similar to that when having a blood sample drawn. You can expect to experience some uterine cramping during the procedure.
Remember…
Amniocentesis and chorionic villus sampling (CVS) are procedures where a sample from the pregnancy is obtained for prenatal diagnostic genetic testing.
Through a diagnostic test, you can learn for sure whether or not your baby has the condition tested positive for by prenatal screening (Down syndrome, trisomy 18, trisomy 13, sex chromosome difference, open neural tube defect).
*CVS cannot detect neural tube defects. Closed neural tube defects may not be detected by amniocentesis.*
These tests are associated with a small chance to lose the pregnancy (miscarriage).
Other genetic conditions can also be detected by these tests.
Your genetic counsellor or prenatal care provider will discuss these testing options with you in more detail and help you to understand the right test for you.
A word about unexpected news
If you have diagnostic testing and the results confirm that your baby has Down syndrome, trisomy 18 or open neural tube defect, genetic counsellors are available to help you discuss your options: continuing the pregnancy, adoption or choosing to end the pregnancy.
Making a decision is not easy. Genetic professionals can help you find resources, such as support groups, that may be helpful to you during and after your decision-making. There are health care practitioners available to help you and offer support no matter what decision you make.
The choice is yours.

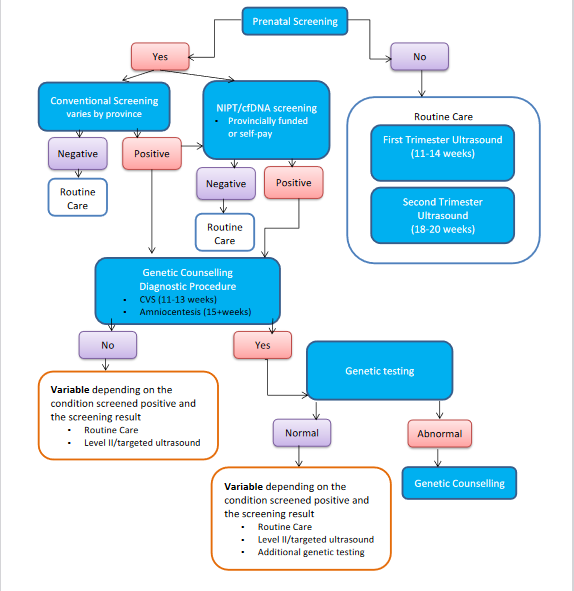
A prenatal screening process map
Online resources
To find your local provincial prenatal screening program go to GECKO > Resources for the Public > Links to provincial programs
For more resources on an Introduction to Genetics, try:
- National Human Genome Research Institute
- Help Me Understand Genetics by the Genetics Home Reference
For more resources on the conditions screened for by prenatal screening, try:
- Canadian Down Syndrome Society
- The Trisomy 18 Foundation
- Support Organization for Trisomy 18, 13 and Related Disorders (SOFT)
- Spina Bifida and Hydrocephalus Association of Canada
- Spina Bifida and Hydrocephalus Association of Canada
- The Association for X and Y Chromosome Variations (AXYS)
- Turner Syndrome Society of Canada
For an appointment with a genetic counsellor at your local genetics centre, you will most likely need a referral from your primary care practitioner or other physician. To locate the nearest centre to you, see Genetics Education Canada: Knowledge Organization (GECKO) https://www.geneticseducation.ca/ Genetics Centres https://geneticseducation.ca/find-your-local-genomics-expert/canadian-clinics
Acknowledgements
This guide was written by a multidisciplinary team and with input from new parents. We are always updating and revising our resources. If you have feedback for us, please do reach out to GECKO@cheo.on.ca
All images are open-source. Links to their original site are attached to each photo
Additional resources
Introduction to genetics and prenatal testing after a diagnostic test (chorionic villus sampling (CVS) or amniocentesis).
Introduction to genetics
Each cell of the body, be it a hair, liver, or heart cell, contains an individual’s genetic information. Genetic information is like a blueprint, containing all the necessary instructions to build a person and for the lifelong growth and development of that individual.
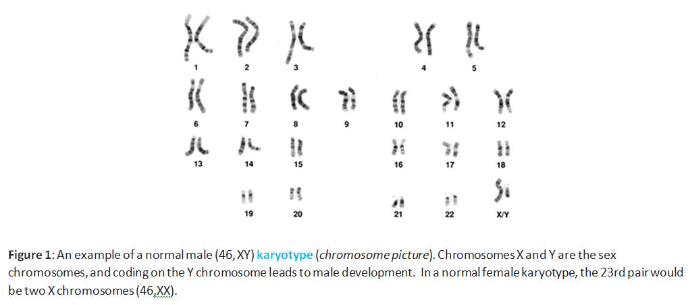
Genetic information is packaged into structures called chromosomes. Typically, inside each cell there are 23 pairs of chromosomes (e.g. two copies of chromosome 1, two chromosome 2, etc.), for a total of 46 chromosomes in each cell (Figure 1). One chromosome from each pair is inherited from each genetic parent.
Mature egg and sperm cells typically have only 23 chromosomes. When an egg cell and a sperm cell mature, they undergo a division process into two identical daughter cells, and each chromosome pair separates. One copy from each chromosome pair goes into each new daughter cell (Figure 2a).
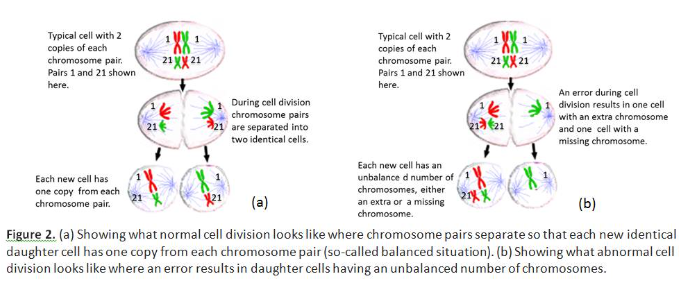
The testes will constantly produce new sperm cells over one’s life. On the other hand, all the eggs the ovaries will ever produce are present at the birth of that individual. These eggs are ‘frozen’ mid-division and, at ovulation, typically one egg will fully divide. These eggs age as the individual ages. Over time, there is an increased chance for there to be an error in the division process, where a chromosome pair does not separate correctly (Figure 2b). In this case the egg contains an extra or missing chromosome. There is nothing that an individual can do to cause or to prevent this. While there is a chance to have a baby born with a chromosome difference at any age; this chance increases as the eggs age (Table 3). An example of a chromosome condition is Down syndrome. An individual with Down syndrome has an extra copy of chromosome 21 (trisomy 21, three copies of chromosome 21) and has 47 chromosomes in total.
A chromosome may contain hundreds to thousands of genes. Genes are the individual instructions to make important proteins for a healthy individual. For example, insulin is an important protein the body makes to control sugar levels. The gene, or instruction, for insulin is located on chromosome 11. There are about 20,000 genes in total and it is important to have the right number of genes and the right set of instructions for healthy growth and development.
Table 3. Pregnant person/egg donor’s (in the case of donated egg) age at delivery and the chance to have a baby with Down syndrome and other chromosome conditions.
Pregnant person/egg donor’s age (Years)Chance to have a baby with Down SyndromeChance of any chromosome condition including trisomy 18 and Down Syndrome
| 20 | 1 in 1,484 (~0.1%) | 1 in 530 (~0.2%) |
| 25 | 1 in 1,362 (~0.1%) | 1 in 480 (~0.2%) |
| 30 | 1 in 994 (~0.1%) | 1 in 390 (~0.3%) |
| 35 | 1 in 403 (~0.3%) | 1 in 180 (~0.6%) |
| 40 | 1 in 98 (~1%) | 1 in 65 (~0.2%) |
| 45 | 1 in 38 (~3%) | 1 in 19 (~5%) |
Diagnostic tests
You can read about the procedures to obtain a prenatal sample in the previous section Diagnostic procedures but what about the testing that is performed on that sample?
Quantitative fluorescence PCR (QF-PCR)
QFPCR is a laboratory test used to precisely measure the amount of DNA present. This test may also be called Rapid Aneuploidy Detection (aneuploidy, refers to genetic conditions< where there are extra or missing whole chromosomes) or RAD. Generally, this is the first test performed on a prenatal sample (amniotic fluid or chorionic villus sample). This test can tell accurately whether the baby has or does not have Down syndrome, trisomy 18, trisomy 13 or a sex chromosome difference. This is the recommended diagnostic test for pregnancies where there is an increased risk for one of the above-mentioned chromosome conditions. Results from this test are usually available within one week.
Fluorescent in situ Hybridization (FISH)
FISH is a laboratory technique used to visualize pieces of DNA. FISH uses small pieces of DNA that are labelled with glowing (fluorescent) tags. These tagged pieces of DNA (probes) will attach to specific parts of specific chromosomes. Like QFPCR, FISH is a technique used to measure DNA. For example, a probe is designed to attach to chromosome 21, if the sample is from someone who has Down syndrome then three probes will attach to the three copies of chromosome 21. If the sample is from someone who does not have Down syndrome then only two probes will attach. This test will tell for certain whether the baby has or doesn’t have Down syndrome, trisomy 18, trisomy 13 or a sex chromosome difference. Results from this test are usually available within one week.
Karyotype
Karyotyping is a laboratory technique used to examine all the chromosomes, evaluating whether there are any major chromosomal differences, including whole extra or missing chromosomes, large extra or missing pieces of a chromosome and structural changes in the chromosomes (e.g. chromosomes that are stuck together or that have exchanged large pieces). Karyotype testing will follow an abnormal result reported by QFPCR or FISH. Results from this test usually take about 2-3 weeks.
Chromosomal Microarray
Chromosomal microarray (CMA) is a newer technology that has recently been added to the prenatal testing menu. In addition to looking at extra or missing whole chromosomes, CMA will also detect very tiny extra or missing pieces of genetic information (microduplications/microdeletions). The potential for complex results and the detection of both unexpected and uncertain findings warrants the need for comprehensive genetic counselling before and after undergoing this test.
Multigene panel
This is a genetic test that reads through multiple genes, letter by letter, at the same time. Gene panels contain carefully selected genes that are known to be associated with specific health, physical or developmental issues, such as a gene panel for epilepsy, for heart conditions or for dwarfism (skeletal dysplasia). A multigene panel may be considered when your genetic health professional suspects a genetic condition.
Whole exome sequencing and whole genome sequencing
This is the latest genetic test that involves reading through all the genes at the same time, all 20,000. The exome refers to the part of the genes that are actually read to make the protein, coding region. The exome makes up only about 1% of all the genetic information. The other part of the genes are not read to make the protein, non coding regions. These parts are called introns. Whole exome sequencing is testing that reads through all the coding regions of the genes. Whole genome sequencing is testing that reads through all the coding and non-coding regions of the genes.
Clinicians who wish to learn more about genetic tests and results can take a look at our resources which go into much more details.
The National Human Genome Research Institute has more resources on genetics/genomics and testing for the public and keen learners.


