Download the comprehensive GECKO Messenger, the quick reference GECKO on the run, and/or the point of care Triage and Surveillance Tool.
Last updated March 2019
Bottom line: Hereditary hemochromatosis (HH) is a common inherited predisposition to absorb excess iron from one’s diet; most individuals with the predisposition do not develop clinical disease. However, HH has the potential to cause morbidity and mortality.
Genetic testing should be considered for:
Adults with biochemical evidence of iron overload (>45% transferrin saturation (TS) and >300mµ/L serum ferritin (SF) in men and post-menopausal women or >200mµ/L SF in pre-menopausal women)
Any adult whose first-degree relative has the C282Y HFE gene mutation
What is HH?
Hereditary Hemochromatosis (HH) can be caused by mutations in different genes. Mutations in the HFE gene are the most common cause of adult onset iron overload1,2. This GECKO Messenger deals EXCLUSIVELY with HFE-associated HH.
Mutations in the HFE gene alter the regulation of iron absorption through the mucosal lining of the gastrointestinal tract. In some predisposed individuals, excessive iron absorption and subsequent storage in various organs (Table 1) eventually lead to cellular injury. If untreated, over time this can cause irreversible damage and shorten life expectancy. With early identification of at-risk individuals, proper surveillance of iron indices, and treatment when necessary, all complications can be avoided.
Table 1. Organs at risk of damage due to excessive iron storage3.
| Organ | Damage |
| Liver | Hepatomegaly, cirrhosis, hepatocellular carcinoma |
| Pancreas | Diabetes mellitus |
| Heart | Dilated cardiomyopathy, congestive heart failure +/- arrhythmia |
| Joints | Arthritis |
| Skin | Hyperpigmentation |
| Testes | Hypogonadism |
While any of these health concerns can be caused by HH, the presence of two or more should greatly increase suspicion that the condition is present.
What do I need to know about the genetics of HH?
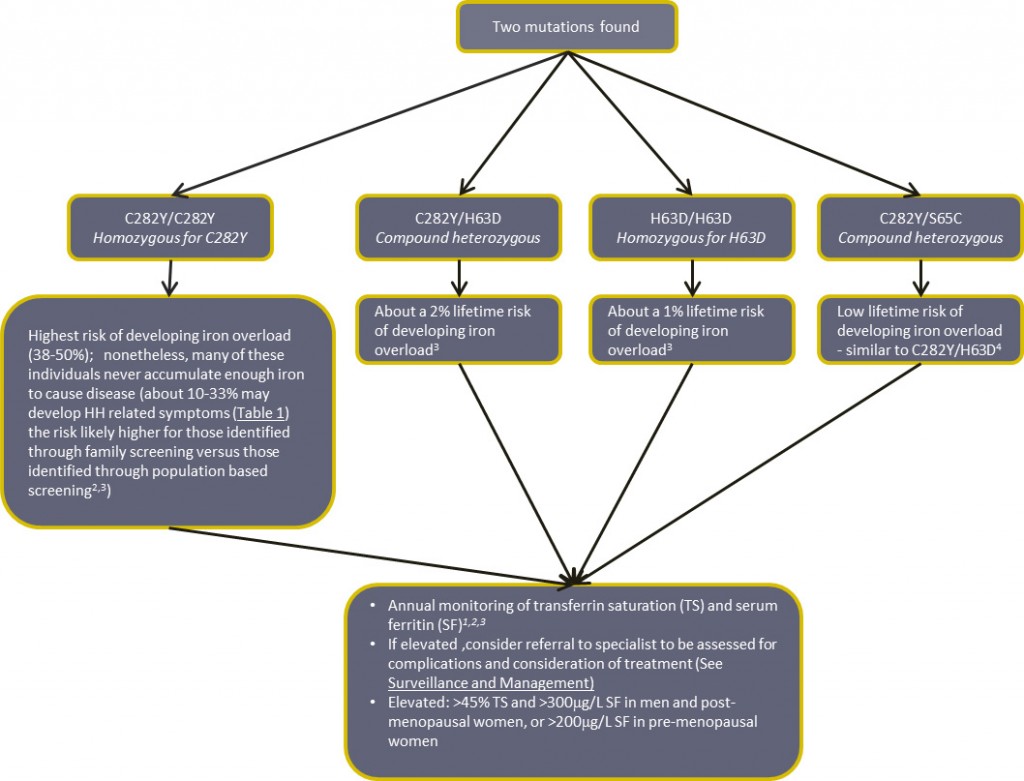
Inherited HH is most commonly caused by mutations in the HFE gene on chromosome 6. Standard testing by North American molecular genetics laboratories is targeted mutation analysis to look specifically for the two most common HFE mutations, C282Y and H63D. These mutations account for over 90% of HH3. Some, but not all, laboratories also test for a rare HFE gene mutation, S65C, which predisposes to iron overload when combined with C282Y similarly to H63D4.
Pattern of inheritance
Autosomal recessive
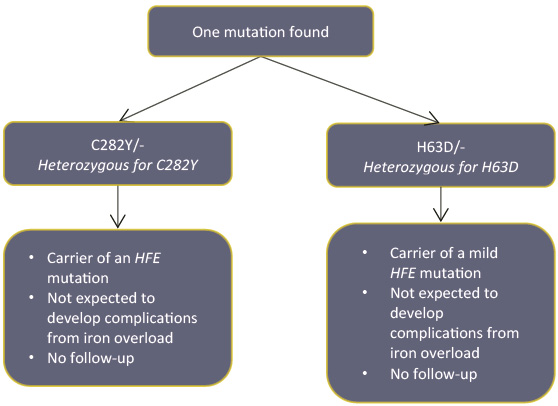
- An individual who has inherited two mutations in the HFE gene, one from each parent, has the predisposition to develop iron overload.
- A person with a single mutation is called a ‘carrier’ and is not at risk of iron overload.
How common is HFE-HH?
About 1 in 3 individuals of northern European ancestry are carriers (heterozygotes) of the C282Y or H63D HFE gene mutations3. About 1 in 260 individuals have two copies of (are homozygous for) the C282Y HFE gene mutation (genotype C282Y/C282Y)2. The prevalence of HFE-HH in other ethnicities is lower.
Who should be offered genetic testing?
Genetic Testing should be offered1,2,3:
To adults with biochemical evidence of iron overload (>45% transferrin saturation (TS) and >300µg/L serum ferritin (SF) in men and post-menopausal women or >200µg/L SF in pre-menopausal women)
If your adult patient has a first-degree relative (sibling, parent or child) with one of the following genetic test results:
- C282Y/C282Y (homozygote)
- C282Y/H63D (compound heterozygote)
- C282Y/S65C (compound heterozygote)
- C282Y heterozygote (carrier)
If your patient has unexplained chronic liver disease and increased transferrin saturation (TS)
Individuals with HFE-HH occasionally demonstrate a normal TS and an elevated ferritin. If clinical suspicion is high and/or the patient has a family history of HFE-HH, genetic testing is still warranted
Who should not be offered genetic testing?
Children do not require genetic testing for HFE-HH. [Please refer to the Canadian Pediatric Society and the Canadian College of Medical Geneticists published guidelines relating to the question of genetic testing of healthy children. For conditions that will not present until adulthood (susceptibility or predictive testing) and where there is no benefit to the child, testing should be deferred until the child is competent to understand the purpose of the test and make an autonomous decision.]
General population screening for HFE-HH is not recommended as the disease penetrance is low1,2.
Who should be offered Biochemical testing for iron overload?
If your patient has suggestive symptoms, physical findings or a family history of HH, transferrin saturation and serum ferritin are ideally ordered together to determine the likelihood of iron overload.
Transferrin saturation (TS)
TS is a reliable screen for iron overload and does not vary with age or the presence of clinical findings. A fasting TS of greater than 45% is considered a sensitive but not specific threshold for identifying individuals who may have iron overload. TS should be performed on a fasting sample as the result can be falsely elevated if a patient has not been fasting.
Serum ferritin (SF)
Normal ranges for SF vary with gender and age and vary slightly from lab to lab. In combination with persistent elevation of fasting TS, ferritin levels of greater than 300mg/ml in men or post-menopausal women and greater than 200mg/mL in pre-menopausal women are suspicious for iron overload.
Remember that SF is an acute phase reactant that can be elevated by other inflammatory processes. Therefore an elevated SF does not necessarily imply iron overload and is not a reliable first or only screen.
What does the genetic test result mean?
The actual risk to develop iron overload is dependent on how many and which gene mutations have been inherited, in addition to other genetic and non-genetic factors.
Click to see what your patient’s genetic test result means:
Patient has two HFE gene mutations
Patient has one HFE gene mutation
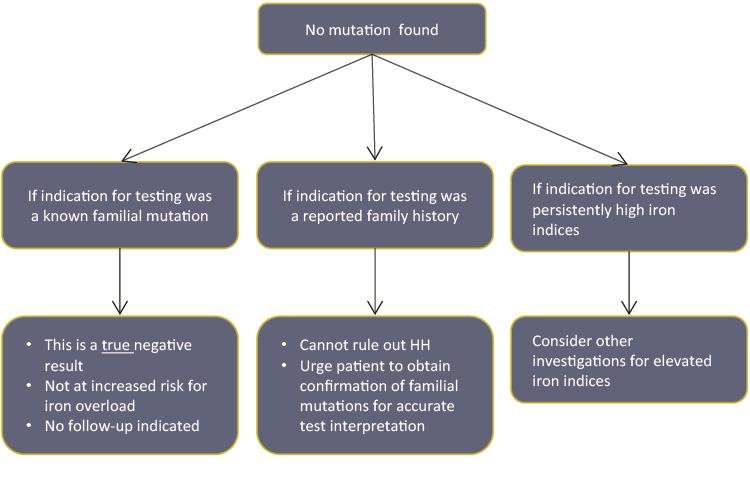
Patient has no HFE gene mutation
Other considerations:
Women are less likely to develop iron overload as a result of menstruation and pregnancy1,2,3
Iron overload due to HFE mutations does not occur in childhood1,2,3
Typically, symptoms of HH present in men aged 40 to 60 and in post-menopausal women; however, onset is variable and can occur much earlier or much later3
Early symptoms are nonspecific and include weakness, lethargy, joint pain and/or stiffness, and abdominal pain with or without hepatomegaly3
Before the onset of symptoms, biochemical evidence of iron overload will be present: >45% transferrin saturation (TS) and >300mµ/L serum ferritin (SF) in men and post-menopausal women, or >200mµ/L SF in pre-menopausal women 1,2,3
Alcohol consumption can exacerbate iron overload and HH- related liver disease3
How do I order the genetic test?
Genetic testing is performed on a blood sample. Click here to find your closest molecular genetics laboratory and the requisition to order testing. These laboratories prefer that you attach their requisition to the Ministry of Health requisition but you can use the MOH requisition alone if necessary.
It is important to include the following information on any requisition for the best test interpretation:
Indication for testing e.g. ‘symptoms of indicated disease’ or ‘abnormal iron indices’ or ‘positive family history’
Ethnicity e.g. Northern European
Relevant family history e.g. parent/sibling with HH (include genetic test results of affected individual if known)
Relevant medical history/investigations; e.g. biochemical iron overload
Where do I refer my patient?
Click here to find your local genetics clinic.
You might refer to genetics if your patient has had a positive genetic test result and would like genetic counselling to discuss the implications for self and family.
Note that genetics clinics vary with regard to the referrals they choose to accept. You may want to contact your local centre for more information.
Include all relevant information on your referral (e.g. family history, genetic test results, and investigations like iron indices) to prevent unnecessary delays due to further clarification needed before an appointment can be booked.
How will genetic testing help you and your patient?
If mutations are identified
- Appropriate Surveillance and Management of the risk of iron overload can be initiated
If no mutations are identified
- If your patient was tested because of a known family mutation, he/she no longer needs frequent monitoring of iron indices and is not at increased risk to develop iron overload. The test has ruled out HH.
- If your patient was tested because of a reported positive family history, more information is needed before ruling out HH in this individual. Your patient should be encouraged to obtain confirmation of the familial mutations and/or diagnosis.
- If your patient was tested because of persistently high iron indices, additional investigations should be considered
Are there harms or limitations of genetic testing?
Limitation: Targeted mutation analysis
- Not every HFE gene mutation is looked for, however, the most common mutations account for more than 90% of all mutations, thus fewer than 10% will be missed using current testing strategies.
Potential harm: Insurance discrimination
- Genetic testing in an asymptomatic individual may challenge his/her ability to obtain life, disability, critical illness, long-term care and/or extended health insurance. However, while this is true of all genetic diseases, HH is a treatable condition and some insurance companies will not deny coverage to a treated individual.
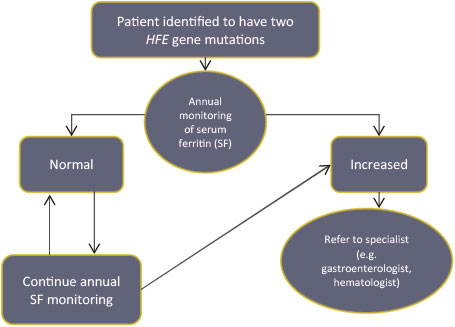
Surveillance and Management
Care map for surveillance and management of your patient identified to have two HFE gene mutations. (Adapted from [2])
Treatment is usually initiated and monitored by a specialist (e.g. haematologist or gastroenterologist). Therapeutic phlebotomy, which is safe and effective, is the mainstay of treatment for iron overload. Treatment is usually indicated in the presence of biochemical evidence of iron overload, symptoms (Table 1 in What is HH?), end-organ damage, and/or a SF of 1000 mµ/L or greater.1,2,3
Iron, cast-iron cooking utensils and vitamin C supplements should not be used by those at risk for, and those with, iron overload. Raw and undercooked shellfish should be avoided because they may carry bacteria that thrive on iron. Dietary iron modification does not significantly alter SF levels and is not a substitute treatment for individuals with iron overload.1,2,3
Individuals with two HFE gene mutations should consider the hepatitis A&B vaccines3.
Resources for health professionals
[1] Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS, American Association for the Study of Liver Diseases. 2011. Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 54:328–43
[2] European Association for the Study of the Liver. 2010. EASL clinical practice guidelines for HFE hemochromatosis. J Hepatol. 53:3–22
[3] GeneReviews. HFE-Associated Hemochromatosis. http://www.ncbi.nlm.nih.gov/books/NBK1440/ Updated April 19th, 2012 [Accessed February 2013]
Expert-authored, peer-reviewed, current disease descriptions that apply genetic testing to the diagnosis, management, and genetic counseling of patients and families with specific inherited conditions.
[4] Wallace DF, Walker AP, Pietrangelo A, Clare M, Bomford AB, Dixon JL, Powell LW, Subramaniam VN, Dooley JS. 2002. Frequency of the S65C mutation of HFE and iron overload in 309 subjects heterozygous for C282Y. J Hepatol. 36(4):474-9.
Gene Messenger. November 2010. HFE-related Hereditary Hemochromatosis http://www.cfp.ca/content/suppl/2009/01/13/55.1.53.DC1/Hemochromatosis_ud.pdf Collection of short reviews on genetics topics designed by a team family physicians, genetic counsellors and geneticists.
Moore AM, Richer J, Canadian Paediatric Society Bioethics Committee. Genetic testing and screening in children. Paediatr Child Health. 2022 Jul 18;27(4):243-253. PMID: 35859682; https://cps.ca/en/documents/position/genetic-testing
Resources for patients and the public
Canadian Hemochromatosis Society. Established to create awareness about the disorder. Additionally provides information and support. www.cdnhemochromatosis.ca [Accessed October 2012].
Authors: S Morrison MS CGC, JE Allanson MD FRCPC, GE Graham MD FRCPC and JC Carroll MD CCFP
Disclaimer:
· GECKO is an independent not-for-profit program that does not accept support from commercial or non-academic entities.
· GECKO aims to aid the practicing non-genetics clinician by providing informed resources regarding genetic/genomic conditions, services and technologies that have been developed in a rigorous and evidence-based manner with periodic updating. The content on the GECKO site is for educational purposes only. No resource should be used as a substitute for clinical judgement. GECKO assumes no responsibility or liability resulting from the use of information contained herein.
· All clinicians using this site are encouraged to consult local genetics clinics, medical geneticists, or specialists for clarification of questions that arise relating to specific patient problems.
· All patients should seek the advice of their own physician or other qualified clinician regarding any medical questions or conditions.
· External links are selected and reviewed at the time a page is published. However, GECKO is not responsible for the content of external websites. The inclusion of a link to an external website from GECKO should not be understood to be an endorsement of that website or the site’s owners (or their products/services).
· We strive to provide accurate, timely, unbiased, and up-to-date information on this site, and make every attempt to ensure the integrity of the site. However, it is possible that the information contained here may contain inaccuracies or errors for which neither GECKO nor its funding agencies assume responsibility.