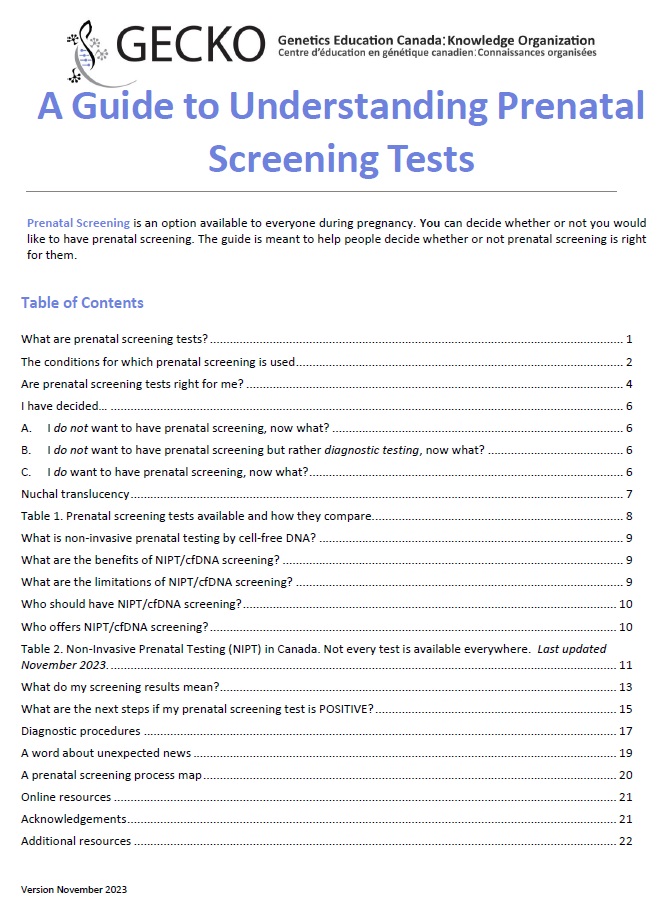
Please find the Updated (Nov 2023) PDF version here (content below will be updated shortly).
Prenatal Screening is an option available to everyone during pregnancy.
You can decide whether or not you would like to have prenatal screening. The guide is meant to help people decide whether or not prenatal screening is right for them.
In Canada, about 1 in 25 (4%) babies is born with a difference, called a congenital anomaly, that may require medical or surgical intervention. The most common differences are structural heart defects, cleft lip and/or palate or a pattern of difference such as Down syndrome. Some risk factors, like family history or pregnant person/egg donor’s, can increase the chance that a person will have a baby with a congenital anomaly. If you have any concerns about your family history, for example you have a genetic condition, there are close relatives with intellectual disability or who were born with one or more congenital anomalies, young children or babies that passed away unexpectedly, be sure to discuss that with your health care provider.
Through available prenatal screening and detailed second trimester ultrasound, the chance to have a baby with some specific genetic conditions or developmental differences present at birth can be more precisely determined.
Prenatal screening is about risk assessment.
If you have any difficulty viewing the content below, you may wish to update or change your web browser, or you may download/view the print friendly PDF version.